In recent years, the Health Resources and Services Administration (HRSA) and the Centers for Disease Control and Prevention (CDC) have articulated a vision of how their work can impact the broader determinants of health (Frieden, 2010; HRSA, 2010). To understand how this work can be accomplished within and between the agencies, it is important to understand the current organization of each agency and how funding flows into and through their networks. This appendix provides a brief overview of each agency and reviews their macro-level funding streams as they relate to primary care and public health opportunities.
WITHIN THE CONTEXT OF THE DEPARTMENT
OF HEALTH AND HUMAN SERVICES
The Department of Health and Human Services (HHS) is the principal agency charged with protecting the health of all Americans, and in fiscal year 2010, it spent $854 billion in pursuit of that goal (see Table A-1 for details). It is notable that together, HRSA and CDC account for less than 2 percent of the department’s budget. In contrast, the National Institutes of Health accounts for 3.65 percent of the HHS budget, the Administration for Children and Families for 6.1 percent, and the Centers for Medicare & Medicaid Services (CMS) for fully 86.5 percent (HHS, 2011).
While HRSA and CDC operate on less than 0.5 percent of total federal outlays, they are responsible for the provision of primary care for tens of millions of vulnerable individuals and for oversight of the public health of the nation, respectively, and thus are positioned to facilitate the integration
TABLE A-1 HHS Outlays by Operating Division (Fiscal Year 2010)
| Operating Division | Outlays (in millions of $) | Percentage of Total Outlays |
|
Centers for Medicare & Medicaid Services |
732,896 |
85.80 |
|
Administration for Children and Families |
56,370 |
6.60 |
|
National Institutes of Health |
33,052 |
3.87 |
|
Health Resources and Services Administration |
8,569 |
1.00 |
|
Centers for Disease Control and Prevention |
6,957 |
0.81 |
|
Public Health and Social Services Emergency Fund |
4,890 |
0.57 |
|
Indian Health Service |
4,350 |
0.51 |
|
Substance Abuse and Mental Health Services |
3,325 |
0.39 |
|
Food and Drug Administration |
2,117 |
0.25 |
|
Administration on Aging |
1,512 |
0.18 |
|
Program Support Center |
575 |
0.07 |
|
Departmental Management |
497 |
0.06 |
|
Agency for Healthcare Research and Quality |
80 |
0.01 |
|
Office of the National Coordinator |
115 |
0.01 |
|
Medicare Hearings and Appeals |
64 |
0.01 |
|
Office of Inspector General |
91 |
0.01 |
|
Office for Civil Rights |
34 |
0.00 |
|
Prevention and Wellness |
10 |
0.00 |
|
Health Insurance Reform Implementation Fund |
21 |
0.00 |
|
World Trade Center Health Program Fund |
0 |
0.00 |
|
Offsetting Collections |
–1,351 |
–0.16 |
|
Total Health and Human Services |
854,174 |
100.00 |
SOURCE: HHS, 2011.
of primary care and public health. Yet, while they share certain objectives, HRSA and CDC are two very different agencies, and located more than 600 miles apart; they have very different responsibilities for fostering the health of the U.S. population.
Among HHS agencies, HRSA and CDC have especially important roles to play in improving population health. HRSA plays a strategic role in helping to ensure access to health services for uninsured and vulnerable populations. Among its other activities, it provides funding to support the provision of primary care services at community health centers, Ryan White clinics, and rural health clinics, as well as training programs for the primary care workforce and maternal and child health care programs. And with its focus on health promotion, prevention, and preparedness, CDC is recognized as a global leader in public health. The agency works with local and state health departments on a number of efforts, including implementing disease surveillance systems, preventing and controlling infectious and
chronic diseases, reducing injuries, eliminating workplace hazards, and addressing environmental health threats. This appendix examines HRSA and CDC in greater detail.
HEALTH RESOURCES AND SERVICES ADMINISTRATION
Established in 1980, HRSA is the primary federal agency responsible for ensuring access to health care services for people who are uninsured, isolated, or medically vulnerable, including those living with HIV/AIDS, mothers and children, and those living in rural areas. HRSA’s vision is “Healthy Communities, Healthy People,” and its mission is “to improve health and achieve health equity through access to quality services, a skilled health workforce and innovative programs” (HRSA, 2011a). HRSA has established four goals to help achieve its vision and mission: to improve (1) access to quality care and services, (2) the health workforce, (3) healthy communities, and (4) health equity (HRSA, 2011a).
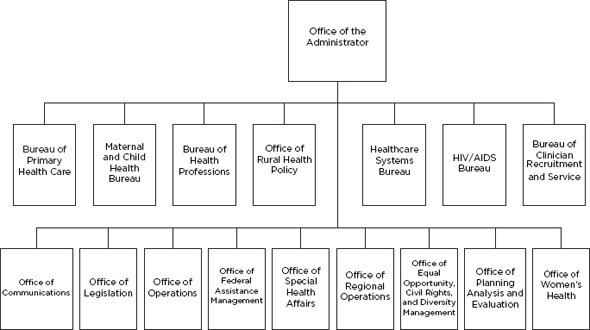
At its highest level, HRSA is organized into 6 bureaus and 10 offices (Figure A-1) (HRSA, 2011c). Each bureau provides clinical and preventive services to vulnerable populations. For instance, the Bureau of Primary Health Care funds health centers in underserved communities that provide comprehensive primary and preventive health care for medically underserved populations regardless of their ability to pay (HRSA, 2011b), while the Maternal and Child Health Bureau functions to improve the health of mothers, infants, and children and aims to reduce health disparities relating to such issues as infant mortality, access to pre-and postnatal care, and health care for children with special health care needs (HRSA, 2011d).
Among other efforts, HRSA functions to improve health by funding health care initiatives and systems such as health clinics, maternal and child health initiatives, and workforce programs including training and loan reimbursement programs. HRSA supports 70 programs that provide funding to such entities as academic institutions, community health centers, public health departments, and local communities. HRSA programs and their funding share some key features. HRSA programs include few flexible funding sources and include only one block grant—the Maternal and Child Health Block Grant. In contrast with the CDC programs discussed below, 10 of the HRSA programs allocate funds based on a formula, and 12 of the HRSA project grants are funded through cooperative agreements which allows HRSA to be substantially involved in local activities. Despite this variability, the majority of HRSA awards are project grants designated for a specified use or project (Federal Funds Information for States, 2011).
Additionally, HRSA programs have some specific funding restrictions. Fifteen of the programs impose some type of matching requirement, and 22 have a maintenance-of-effort provision. These may require that additional
TABLE A-2 HRSA Fiscal Year 2010 Budget Authority
|
Activity |
Funding Level (in millions of $) |
Percent of Total |
|
HIV/AIDS |
2,315 |
30.90 |
|
Primary Care |
2,253 |
30.07 |
|
Health Workforce |
1,230 |
16.42 |
|
Maternal and Child Health |
984 |
13.13 |
|
Other Activities |
837 |
11.17 |
|
Health Care Systems |
267 |
3.56 |
|
Rural Health |
185 |
2.47 |
|
Less Funds from Other Sources |
–579 |
–7.73 |
|
TOTAL |
7,492 |
100.00 |
SOURCE: HHS, 2011.
funds be generated by the program or through other grants. Many of these programs have a supplantation provision requiring that the grantee use the funds to supplement, not supplant, existing funding for specified grant activities. These provisions are in addition to funding restrictions, such as on the use of funds for the delivery of health care services, indirect costs, and facility construction (Federal Funds Information for States, 2011).
In fiscal year 2010, HRSA was appropriated $7.5 billion (Table A-2). It received nearly equal funding for its HIV/AIDS and primary care initiatives (30.9 and 30.1 percent, respectively), while 16 percent of its funding was dedicated to health workforce development and maintenance (HHS, 2011).
CENTERS FOR DISEASE CONTROL AND PREVENTION
Established in 1942, CDC is perhaps the most well known of Department of Health and Human Services (HHS) agencies. The agency pursues its mission of “Health Protection … Health Equity” through collaboration with nationwide and global partners to “monitor health, detect and investigate health problems, conduct research to enhance prevention, develop and advocate sound public health policies, implement prevention strategies, promote healthy behaviors, foster safe and healthful environments, and provide leadership and training” (CDC, 2010).
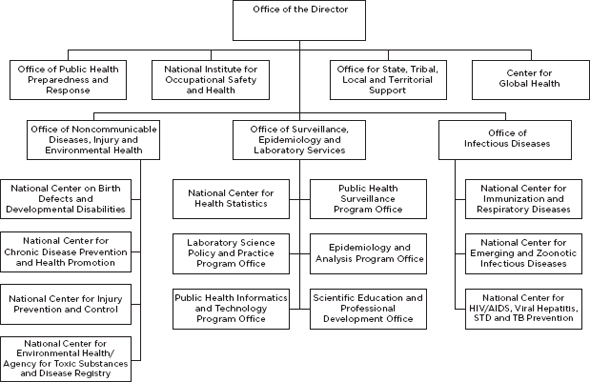
At its highest level, CDC is organized into five offices, the Center for Global Health, and the National Institute for Occupational Safety and Health (Figure A-2). Three of these offices—the Office of Infectious Diseases; the Office of Noncommunicable Disease, Injury, and Environmental Health; and the Office of Surveillance, Epidemiology and Laboratory Services—are further divided into national centers and program offices (CDC, 2011b). These centers and offices are further partitioned into divisions
and then branches, which are narrowly focused on health topic areas. For instance, the National Center for Chronic Disease Prevention and Health Promotion comprises nine divisions: the Division of Adolescent and School Health; the Division of Cancer Prevention and Control; the Division of Adult and Community Health; the Division of Diabetes Translation; the Division of Nutrition, Physical Activity and Obesity; the Division of Reproductive Health; the Office of Smoking and Health; the Division for Heart Disease and Stroke Prevention; and the Division of Oral Health (CDC, 2011a). Each division, center, and office is headed by a director who ultimately reports to the director of CDC and the secretary of HHS.
CDC functions to improve the health of all Americans through various public health initiatives, such as vaccine promotion, infectious disease prevention, and management of chronic disease. While organizing many of its own campaigns, CDC functions largely through its grant-making programs. These programs cover a broad spectrum and share several features. Only one program—the Preventive Health and Health Services Block Grant—provides flexible funding to states that can be used for a variety of activities, from clinical services to data surveillance. The remaining CDC programs provide funding through project grants, whereby the funding is competitive and restricted to a specified use or project. Twenty-nine of these project grants operate as cooperative agreements between the federal government and recipient(s) (Federal Funds Information for States, 2011).
Programs in the CDC inventory also are similar in their funding restrictions. Most have general restrictions that apply to all CDC grants. These restrictions generally entail use limitations, which allow funding only for reasonable program costs and exclude the use of funds for the purchase of equipment and construction and for rehabilitative services or clinical care. These restrictions also require the recipient to play a substantial role in carrying out the project objectives and do not allow for the reimbursement of pre-award costs. In addition to these general restrictions, some programs impose matching or maintenance-of-effort requirements. For example, state health departments must match $1 for every $4 they receive under cooperative agreements for state-based diabetes control programs and evaluation of surveillance systems. Additionally, while some programs have specific maintenance-of-effort requirements, others have supplantation provisions (Federal Funds Information for States, 2011).
In fiscal year 2010, CDC was appropriated nearly $6.5 billion in discretionary funds (Table A-3). At 23.5 percent, the largest portion of this funding was dedicated to public health preparedness and response. This was followed by funding for prevention of HIV/AIDS, viral hepatitis, sexually transmitted diseases (STDs), and tuberculosis (17.3 percent) and $949 million for chronic disease prevention and health promotion (HHS, 2011). The primary uses of these funds are to support public health through state
TABLE A-3 CDC Fiscal Year 2010 Budget Authority
|
Activity |
Funding Level |
Percent of Total |
|
Public Health Preparedness and Response |
1,522 |
23.51 |
|
HIV/AIDS, Viral Hepatitis, STD, and TB Prevention |
1,119 |
17.28 |
|
Chronic Disease Prevention and Health Promotion |
949 |
14.66 |
|
Immunization and Respiratory Diseases |
721 |
11.14 |
|
Public Health Scientific Services |
441 |
6.81 |
|
Occupational Safety and Health |
430 |
6.64 |
|
Business Support Services |
367 |
5.67 |
|
Global Health |
354 |
5.47 |
|
Emerging and Zoonotic Infectious Diseases |
281 |
4.34 |
|
Public Health Leadership and Support |
194 |
3.00 |
|
Environmental Health |
181 |
2.80 |
|
Injury Prevention and Control |
149 |
2.30 |
|
Child Health, Disabilities, and Blood Disorders |
144 |
2.22 |
|
Preventive Health and Health Services Block Grant |
100 |
1.54 |
|
Agency for Toxic Substances and Disease Registry |
100 |
1.54 |
|
Buildings and Facilities |
69 |
1.07 |
|
User Fees |
2 |
0.03 |
|
Less Funds from Other Sources |
–649 |
–10.02 |
|
TOTAL |
6,474 |
100.00 |
NOTE: STD = sexually transmitted disease; TB = tuberculosis.
SOURCE: HHS, 2011.
and local health departments and to sponsor nationwide public health research and programming.
REFERENCES
CDC (Centers for Disease Control and Prevention). 2010. About CDC: Vision, mission, core values, and pledge. http://www.cdc.gov/about/organization/mission.htm (accessed November 1, 2011).
CDC. 2011a. Chronic disease prevention and health promotion: Organizational chart. http://www.cdc.gov/chronicdisease/about/org_chart.htm (accessed November 1, 2011).
CDC. 2011b. Department of Health and Human Services Centers for Disease Control and Prevention (CDC). http://www.cdc.gov/maso/pdf/CDC_Chart_wNames.pdf (accessed November 1, 2011).
Federal Funds Information for States. 2011 (unpublished). Inventory of federal funding streams: A detailed review of HRSA and CDC funds. Washington, DC: Institute of Medicine.
Frieden, T. R. 2010. A framework for public health action: The health impact pyramid. American Journal of Public Health 100(4):590-595.
HHS (Department of Health and Human Services). 2011. Advancing the health, safety, and well-being of our people: FY 2012 president’s budget for HHS. Washington, DC: HHS.
HRSA (Health Resources and Services Administration). 2010. Public Health Steering Committee recommendations (draft). Washington, DC: HRSA.
HRSA. 2011a. About HRSA. http://www.hrsa.gov/about/index.html (accessed November 1, 2011).
HRSA. 2011b. Bureau of Primary Health Care. http://www.hrsa.gov/about/organization/bureaus/bphc/index.html (accessed November 1, 2011).
HRSA. 2011c. Bureaus and offices. http://www.hrsa.gov/about/organization/bureaus/index.html (accessed November 1, 2011).
HRSA. 2011d. Maternal and Child Health Bureau. http://www.hrsa.gov/about/organization/bureaus/mchb/index.html (accessed November 1, 2011).