Appendix D
Masticatory System: Anatomy and Function
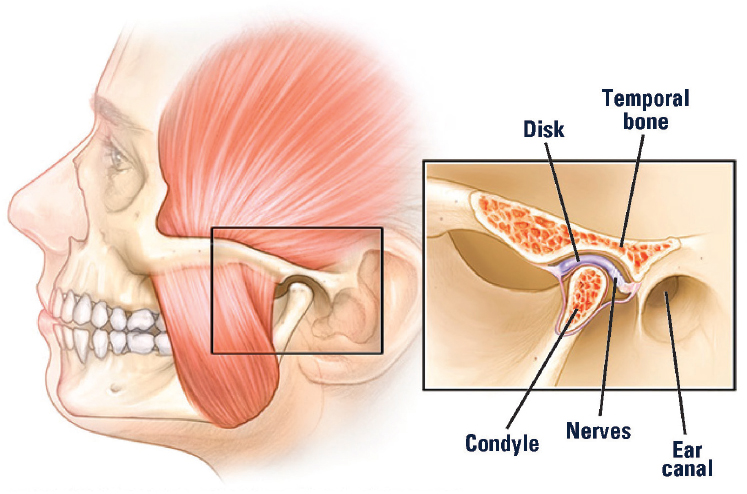
The musculoskeletal structures of the masticatory system and the neurological controls supporting a wide diversity of functions are complex, and much remains to be investigated (Gremillion and Klasser, 2018; see Chapter 4). The following description of the anatomy is intended to highlight the complexity of this system and some of its unique characteristics (see Figure D-1).
BONES
The three major bones of the masticatory system are the maxilla, or upper jaw; the mandible, or lower jaw; and the temporal bone, which is connected to the upper jaw and thereby forms the temporomandibular joint (TMJ) with the mandible. A minor bone, the hyoid, floats beneath the mandible and serves as an attachment point for muscles and ligaments that link the mandible with several other structures. One additional bone, the sphenoid, is fixed between the upper jaw and the temporal bone.
MASTICATORY MUSCLES
The muscles associated with mandibular movement are organized into five groups according to their major functions. Muscles in each group exist and function as pairs, one on the right side and one on the left side of the body:
SOURCE: Mayo Clinic, 2019.
- Primary muscles of mastication: The most recognized group is composed of four muscles that function in pairs and are primarily responsible for TMJ function and mandibular movement. These include the masseter and temporalis muscles, which are responsible for closing the mandible; the medial pterygoid muscle, which is responsible for closing and lateral movements of the mandible; and the lateral pterygoid muscle, which is responsible for opening, deviation to either side, and anterior movement of the jaw. The attachments and orientation of these muscles permit the mandible to function in three planes.
- Accessory muscles of mastication—directly associated with mandibular function: Jaw opening is assisted by sets of paired muscles (including the digastric, geniohyoid, mylohyoid, omohyoid, sternohyoid, sternothyroid, stylohyoid, and thyrohyoid muscles), which coordinate the full integration of mandibular movement during opening and closing through their attachments to the hyoid bone, the mandible, and other bones.
- Accessory muscles—indirectly associated with mandibular function: These muscles are in the cervical area (including the sternocleidomastoid and scalenus anterior, scalenus medius, and scalenus
-
posterior muscles) and attach to the sternum, temporal bone, clavicle, cervical vertebrae 1–7, and ribs 1–2. These muscles stabilize the skull and neck and allow the mandible to move relative to the skull.
- Extrinsic muscles for the tongue: These muscles function to elevate, depress, withdraw, or protrude the tongue.
- Intrinsic muscles within the tongue: These muscles permit the tongue to create shapes (such as curling) and move from cheek to cheek.
Because the jaw moves in three dimensions (resulting in translational [gliding] and rotational movements), the muscle contraction necessary to create movement of the mandible (in particular, for chewing) must occur simultaneously with other contractions of the muscles to control the components of the TMJ. A healthy masticatory system appears to function effortlessly; by contrast, a compromised system can produce pain and dysfunction.
TEMPOROMANDIBULAR JOINTS
TMJs include the rounded end of the mandible (mandibular condyle), the edge of the temporal bone (glenoid fossa), and the articular disc that is positioned between the condyle and fossa. The temporomandibular ligament overlies the joint and provides some lateral stability. The joint itself is surrounded by a capsule that provides a small amount of stability and that also contains the synovial fluid. The synovial fluid provides essential nutrients and lubrication. Without this fluid there would be increased friction and shear stress leading to disc degeneration.
The articular disc, located in the joint capsule, is shaped like a donut but is thinner in the middle and thicker on the edges. The disc is composed of fibrocartilage (which is different from the hyaline cartilage in other joints such as the knee or hip). The articular disc plays a major role in accommodating the movement of the jaw, absorbing shock, and distributing loads. The disc is attached on either side via ligaments to the mandible’s condyle. Blood supply to the joint and surrounding muscles is provided from the external carotid and maxillary arteries and its branches. The central portion of this disc does not contain a blood supply. The anterior and posterior of the disc are not firmly attached to the condyle; rather, these areas are free of firm attachment in order for the disc to pivot as the condyle moves. This lack of attachment may contribute to disc instability.
The articular disc separates the joint into two fluid-filled compartments. Each compartment has a different purpose. The lower compartment (the articular disc, mandibular condyle, and relevant ligaments and other structures) is involved in rotational movements. This rotational movement allows the mandible to move from a closed position to a partially open one.
The upper compartment (the articular disc, temporal bone, and relevant ligaments and other structures) is involved in the translational or gliding motion of the joint, in which the disc slides against the temporal bone and the condyle moves anteriorly down the slope of the joint, allowing further mouth opening. Normal joint motion transitions seamlessly from rotation to translation to provide maximal mouth opening.
In children, the primary growth center for the mandible lies immediately below the fibrocartilaginous lining, making it susceptible to damage from pathological conditions. Throughout an individual’s life-span, the mandibular condyle and the articular disc are capable of adaptive remodeling to accommodate the functional demands of the masticatory system. Losing molars on one side without replacement, for example, will induce adaptive change in the condyles and discs on each side; this adaptive change is typically termed osteoarthrosis. When demands for adaptation exceed the biological capacity of an individual, a complex pattern of breakdown occurs in the cortical bone of the condyle, the articular disc, and the capsular and ligamentous tissues of the joint, which is termed osteoarthritis or degenerative joint disease.
INNERVATION
The innervation of the masticatory muscles (motor) and the TMJ (sensory) is derived from the mandibular branch of the trigeminal nerve, the largest of the cranial nerves. Surrounding tissues are innervated by nerve endings that allow the brain to monitor the effects of movement, which is important in initiating movement and controlling the mechanics of the joint. The sensory innervation of the accessory muscles includes both the trigeminal and cervical nerves. The blood supply to the joint and surrounding muscles is provided from the external carotid and maxillary arteries and their branches.
NEURAL CONTROL
The neurophysiological controls of mandibular sensation and movement are complex. The primary masticatory muscles contain motor units (a group of fibers that contract along with the motor nerve that controls the contraction of all of the fibers in the group) that are intermediate in size (500–1,000 fibers) between the very small units for muscles that control eye movements and the very large units for muscles in the lower limbs. A motor unit in the masseter muscle is about 5 mm in length and height and is interspersed with muscle fibers from other units. Through recruitment of multiple motor units, the masseter muscle can exert very high forces, and, via the small physical size of each unit as well as the initial recruitment of
the motor units with the least number of fibers, the masseter muscle can also exert very low forces with incredible precision, such as during speech. The brain can selectively activate different parts of the primary masticatory muscles in order to achieve the desired movement. This selective activation also occurs as a form of adaptation in response to pain.
Movement is of three forms: voluntary (such as opening or closing the jaw), cyclic (during mastication), and reflex (which contributes to the refined control of both voluntary and cyclic movements). In addition to the motor cortex controlling voluntary mandibular movements, a well-studied area of the brainstem called the central pattern generator controls the cyclic masticatory movements of the jaw, face, and tongue during chewing. These movements are simultaneously under voluntary control. The central pattern generator receives input from the teeth (to protect the teeth from excessive loads), the muscle spindles (for muscle length and rate of change), tendons (as force output from the muscles), and the capsule of the TMJ (for position and load). The central pattern generator is highly adaptive and can respond to immediate changes in food textures and to changes in the dental occlusion over time.
Reflex controls occur at muscle spindles and at brainstem interneurons. Muscle spindles contribute to the control of contraction, velocity, and muscle length. The reflex controls provide, for example, sustained and increasing force in order to bite into a hard food as well as interruptions in the chewing cycle if conditions change, such as encountering unexpected texture in a food bolus or biting the cheek. A jaw-opening reflex would normally be triggered by many of the sensory inputs activated during the closing phase of chewing; the central pattern generator actively suppresses that reflex in order for chewing to occur. Similarly, in response to information from the muscle spindles, a reflex activation of the closing muscles would occur during the rapid opening phase of chewing; the central pattern generator similarly actively suppresses the potential activation of the closing muscles. The presence of pain profoundly alters these internal controls; the muscle coordination decreases, and the reciprocal controls between the opening and closing muscles during the chewing cycles lose their effectiveness, contributing to a degradation of function during both simple movements of opening and closing and complex movements of chewing. Adaptations to these degradations—made so that a person can continue to chew, open, and close the mandible—lead to further demands on the muscles and, eventually, overuse.
The extensive number of orofacial sensory receptors encode peripheral information and inform the brain regarding how the teeth are about to contact or are contacting, the texture of the food bolus, mandibular position, and the acceleration and velocity of mandibular movement. This information serves in a feedback loop to allow further control of movement. The
sensory system is capable of considerable adaptation, such as adjusting to the substantial change in sensory feedback to the brain that comes from dentures and from dental implants (where the normal ligament connecting tooth to bone, which provides sensory information regarding contact to a tooth, has been lost). An older model of motor control suggested that pain exerted a necessary inhibition on motor contraction. However, motivated behavior and coping mechanisms can substantially modify the impact that pain may have in inhibiting movement, and muscle activity can be reorganized to compensate for pain as well. Intense or persistent stimulation from the periphery, such as from trauma to the jaw or sustained stretching of the masticatory muscles, can transform the functioning of second-order neurons into central sensitization, which represents an increased level of excitability to subsequent stimuli. Clinically, this can appear as light touch to the face being experienced as pain, and the hyper-excitability of the nerves also leads to spontaneous activity and pain. The unmasking of neurons that were previously silent occurs with central sensitization, and the brain can misinterpret sensory inputs that may be unrelated to the original injury. These processes can persist even after the original injury heals and can be amplified by other regions of the brain (e.g., by fear of movement or by anxiety). These many processes will affect the functioning of the central pattern generator, altering mastication, leading to further dysregulation in mandibular movement as an attempt to continue to function, and thereby serve as contributing factors for the perpetuation of pain and alteration in TMJ mechanics in temporomandibular disorders.
CERVICAL SYSTEM
The cervical system has a critical role in both normal and abnormal functioning of the TMJ. Head posture, for example, will influence condylar position and therefore the arc of the open and closing movements of the mandible as well as where the upper and lower teeth make first contact. The joint adjacent to the TMJ is the joint between the skull and the first cervical vertebrae, and controlled jaw function requires participation by much more than just the muscles that directly move the jaw. The group of accessory muscles that are indirectly associated with mandibular function attach to the sternum, temporal bone, clavicle, cervical vertebrae 1–7, and ribs 1–2. Their innervation includes C2–C8 and the spinal accessory nerve.
It is notable that the coordination between the masticatory and the cervical systems is substantially altered when pain is present in either system. The presence of a dependency between a masticatory system disorder and other disorders would likely shift the manifestation of the particular masticatory disorder from localized to multi-system.
The stability of a joint is achieved at the expense of the possible range of motion allowed by that joint. Just as in the shoulder, the design of the human TMJ is a balance of structural stability and freedom of movement. The stability of the TMJ is achieved via coordinated action of the muscles of mastication, some of which extend to the chest and to the shoulder. Consequently, healthy function in the TMJ is achieved through a complex layering of muscle activity.
REFERENCES
Gremillion, H. A., and G. D. Klasser, eds. 2018. Temporomandibular disorders: A translational approach from basic science to clinical applicability. Cham, Switzerland: Springer International Publishing.
Mayo Clinic. 2019. TMJ disorders. https://www.mayoclinic.org/diseases-conditions/tmj/symptoms-causes/syc-20350941 (accessed December 31, 2019).
This page intentionally left blank.








