4
Social Infrastructure for Healthy Longevity
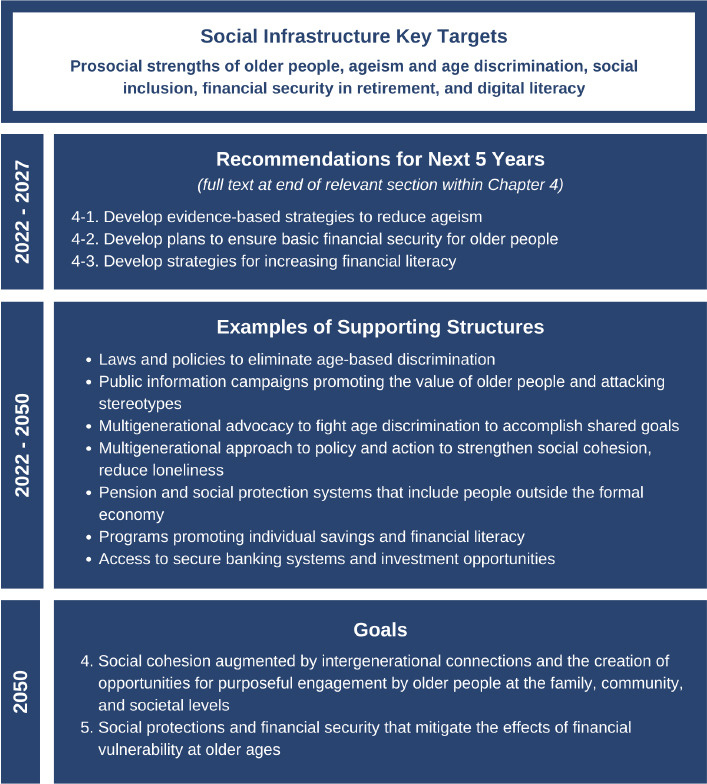
This chapter lays out key targets for achieving the social infrastructure goals for Vision 2050, outlined in Figure 4-1, along with recommendations and supporting structures to assist in that process. The commission believes that building these important aspects of social infrastructure is critical to healthy longevity but must be carried out in conjunction with efforts in the other domains discussed in this report.
For the purposes of this report, the commissioners build on the World Health Organization (WHO) definition of social determinants of health (SDOH) as conditions or circumstances in which people are born, grow, live, work, and age, all of which are shaped by social, economic, and political forces (WHO, 2022b). Ideally, SDOH would directly enable healthy longevity, but national and global social, political, and economic conditions have instead hindered people’s ability to remain healthy as they age. These conditions include unjust economic structures, poorly designed policies and programs, harmful governing practices, unequal shares of social and economic resources, or a combination of all of these factors and more. Consequently, many activists and scholars argue that SDOH are more accurately framed as “social determinants of inequalities in health.” The distribution of resources and opportunities—for health care, education, a healthy living environment, and employment—is fundamental to healthy longevity and is directly impacted, either positively or negatively, by public policy. Hence, this chapter’s focus is on identifying SDOH policies that can drive health and health equity toward realizing the vision set forth in Chapter 2.
This chapter also presents current evidence on key SDOH and their interactions across individual and institutional levels, highlighting programs, structures, and policies that promote equitable outcomes in healthy longevity, along with
relevant case studies. Promising SDOH solutions, if brought to scale, can have far-reaching positive effects for societies worldwide and contribute to global healthy longevity.
The remainder of this chapter describes the key targets that the commission selected based on their ability to catalyze change toward healthy longevity: capitalizing on the prosocial strengths of older people, combating ageism, fostering social inclusion, ensuring financial security in retirement, and achieving digital literacy. The discussion of these key targets draws on evidence and recommendations from international reports, highlighting alignment with related international frameworks. In addition to providing background information, the section on
each key target provides examples of case studies and interventions that show promise for moving toward healthy longevity. Finally, several sections conclude with levers for empowering change, including metrics for assessing the status of progress on the target and research questions to be addressed.
SOCIAL DETERMINANTS OF HEALTH
Understanding and addressing the various types of SDOH across the life course are important goals because experiences in early or young adult life can have long-term implications and determine whether people will age well or poorly and achieve their full potential. These determinants can arise at various points along the life course and may not be directly linked to health or to factors that can be influenced by a health system. The following are examples of SDOH that can affect health and equity (WHO, 2022b):
- “income and social protection;
- education;
- unemployment and job insecurity;
- working-life conditions;
- food insecurity;
- housing, basic amenities, and the environment;
- early-childhood development;
- social inclusion and nondiscrimination;
- structural conflict;
- access to affordable health services of decent quality”; and
- health, financial, and digital literacy.1
Researchers estimate that 10–20 percent of health outcomes are influenced by clinical care (Magnan, 2017), while the remaining 80–90 percent are influenced by SDOH and other related factors, such as health behaviors and the environment. Accordingly, addressing these factors is of critical importance to increasing the potential for global healthy longevity.
This chapter addresses the key targets related to social infrastructure the commission believes are most integral to healthy longevity. Key targets include capitalizing on the prosocial strengths of older people, combating ageism, fostering social inclusion, ensuring financial security, and improving digital literacy. Other SDOH are discussed in Chapters 3, 5, and 6. It is beyond the scope of this report to analyze the effects of all SDOH, so the commissioners prioritized the inclusion of those that are most important to tackle in the near term.
___________________
1 Although health, financial, and digital literacy is not an official determinant listed by WHO, the commission asserts that it is a vital determinant of health equity.
Effects Across the Life Course
Healthy longevity can be achieved only by making changes across the life course. The commission emphasizes the numerous opportunities to improve healthy longevity among younger people, at a time when their actions, experiences, and environmental exposures have a significant influence on their health trajectory across the life course.
Although the key targets in this report are important for today’s older people and, in most cases, all people, other interventions targeting younger people will also be needed to improve healthy longevity for older people of the future. For example, high-quality “early-childhood development and education are key determinants of future health and well-being” (Paris, 2018, p. 16). The advantageous lifelong effects of a supportive and safe childhood and the beneficial role of socioemotional competence in individual health and well-being influence future health. For example, a Jamaica-based study studied outcomes in children who were part of a program in which community health workers taught parenting skills and provided nutritional supplementation over a 2-year period (Gertler et al., 2014). The children who received the intervention realized 25 percent higher earnings 20 years later compared with the control group. Thus, early-childhood development sets the stage for lifelong thriving and is a cost-effective investment that countries can make to improve lifelong health and well-being. While it is beyond the scope of this report to discuss such interventions and their effects in detail, many reports, such as the WHO (2009) report Social Determinants of Health and Well-Being Among Young People, address the relationship between SDOH and younger people.
Poverty prevention, education, secure and safe housing, social support systems, and access to integrated health systems at all ages are also important for ensuring healthy longevity. Structural changes in social policies and practices can help to avoid negative impacts on health that stem from social and economic disadvantage. Public understanding that poor health outcomes and unhealthy aging are socially determined can empower people to demand change from their governments. Medicalizing these social determinants and needs and focusing on them at an individual level will improve health status only for those individuals at that particular point in time. To have a real effect on populations, investments must be made in the community, addressing social needs and risks at the system level, with downstream benefits for the entire community. For example, providing access to food for a patient who presents at a health clinic will help that person for a discrete period of time, whereas ensuring that there are markets in a neighborhood without access to food can help the entire community.
Making systemic investments is key to leveraging an unprecedented opportunity to improve health on a global scale through focused attention on the needs of disadvantaged populations. To represent the relationships between structural drivers and various SDOH and their combined impact on equity, the commission adapted Solar and Irwin’s (2010) conceptual framework (see Figure 4-2).
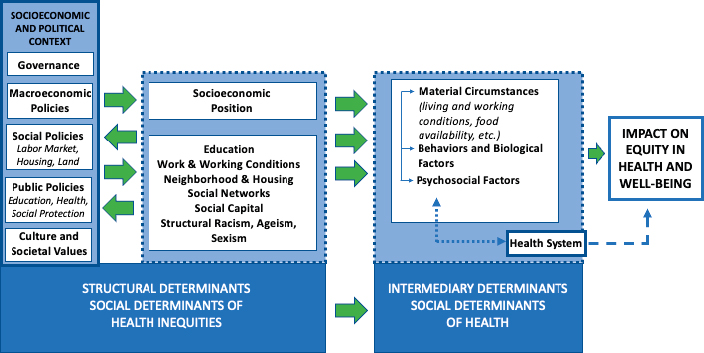
SOURCE: Adapted from A conceptual framework for action on the social determinants of health, Solar and Irwin, 2010.
Impacts of Poverty and Inequality on Life Expectancy
Recent research illustrates the critical importance of certain social determinants for achieving healthy longevity. Life expectancy follows a social gradient, whereby the more deprived an area, the shorter the life expectancy of its population (Marmot, 2020). “Neighborhood deprivation, measured as the proportion of residents with low income, low education, and being unemployed,” is one indication of concentrated inequalities (Bender et al., 2015, p. 2). Researchers studied the effects of neighborhood characteristics in the United States on six common chronic conditions—hypertension, heart problems, stroke, diabetes, cancer, and arthritis. They found that “women living in disadvantaged neighborhoods were more likely than other women to develop heart disease, even after controlling for individual characteristics and aspects of the physical environment (e.g., population density, pollution, walkability)” (Freedman et al., 2011, p. 83). As inequality has persisted, this social gradient has become steeper, and disparities in life expectancy have increased. This is the case in all countries, regardless of income level. For example, a recent review examined life expectancy disparities across regions in England. The study found that for both men and women, life expectancy was lower in the most deprived areas and higher in the least deprived areas. The researchers surmise that “social and economic conditions have undermined health” (Marmot, 2020, p. 10) such that “people living in more deprived areas spend more of their shorter lives in ill health relative to those in less deprived areas” (p. 3).
The United States also has geographic disparities in life expectancy among counties that have increased over the past 35 years (Chetty et al., 2016). Socio-
economic, race, and ethnicity factors alone now explain 60 percent of U.S. life expectancy (Dwyer-Lindgren et al., 2017). Improvements in life expectancy at age 50 in majority Black counties lag nearly 30 years behind counties where fewer than 5 percent of residents are Black (Tan, 2020). “The US reduction in 2020 life expectancy is projected to exceed that of most other high-income countries, indicating that the United States—which already had a life expectancy below that of all other high-income developed nations prior to the pandemic—will see its life expectancy fall even farther behind its peers” (Andrasfay and Goldman, 2021, p. 3). Given the numerous disparities in health and wealth, it is not surprising that declines in life expectancy in the United States are not evenly distributed. Andrasfay and Goldman (2021) estimate that, among Black and Latinx populations, the pandemic will result in life expectancy reductions three to four times greater than reductions among White populations. “[T]he disproportionate burden of death in Black and Latino populations reflect the underlying social disparities that have been documented for decades and amplified during the current pandemic,” demonstrating that social factors are at the root of gross inequalities in health outcomes (Andrasfay and Goldman, 2021, p. 4).
In all countries around the world, growing levels of inequality—measured as the difference between a country’s gross domestic product (GDP) and the distribution of wealth (i.e., the net worth of a person) or income (i.e., the amount of money a person receives on a regular basis) within its population—threaten the achievement of equitable healthy longevity. In 2020, the United Nations’ (UN’s) World Social Report showed increasing income inequality for more than 70 percent of the global population, which hampers economic development in a country (UN, 2020b). Additionally, in 2021, the World Economic Forum noted that, although income inequality among countries has decreased over the past decades, the income inequality within countries has actually increased (Myers, 2021). Gaps in wealth inequality are even higher.
“While in general a country’s life expectancy increases with national income, some countries … achiev[e] higher or lower life expectancy than would be predicted by their per capita income” (Freeman et al., 2020, p. 1). An analysis of Brazil, Ethiopia, and the United States found that Ethiopia had 3 more years of life expectancy than anticipated based on its GDP per capita, and Brazil had 2 more years (Freeman et al., 2020). The researchers attributed the extra 3 years of life expectancy in Ethiopia to “community-based health strategies, improving access to safe water, female education and gender empowerment, and the rise of civil society organisations” (Freeman et al., 2020, p. 1). Conversely, life expectancy in the United States was 2.9 years lower than expected, based on GDP per capita, demonstrating that a country’s national income alone does not dictate life expectancy. Countries can take steps to address identified factors to reduce levels of inequality among residents.
Alignment with the Sustainable Development Goals
Substantial crossover exists between the social and physical environment enablers of healthy longevity and the UN Sustainable Development Goals (SDGs) (outlined in Chapter 2). Countries that strengthen institutional structures to improve healthy longevity will also make progress toward attaining the SDGs. Globally, realizing healthy longevity will require progress on the SDGs of eliminating poverty in older age (SDG 1), ensuring gender equality across the life course (SDG 5), promoting decent work for people of all ages (SDG 8), reducing inequalities and ending discrimination in later life (SDG 10), and building inclusive and accessible communities (SDG 11).
“While action on SDGs is likely to affect health and health equity either directly or indirectly, the effects on inequalities in SDOH will need to be assessed and monitored” (Marmot and Bell, 2018, p. 6). To this end, the implementation of actions to attain the SDGs will need to cut across traditional silos, with attention paid to how action on one goal can impact goals in other areas so governments and other stakeholders can maximize cobenefits. Thus, to collectively accelerate progress toward the SDGs, it will be important to find ways to work across sectors and ensure that action in one sector does not adversely affect others.
Finding 4-1: The social determinants of health have enormous consequences that can influence people’s ability to achieve healthy longevity.
Conclusion 4-1: In designing and implementing policies to promote healthy longevity, it will be essential to acknowledge the cumulative effects of social determinants of health across the life course. With equity at the core of these policies, governments can address the historical and structural inequalities that have translated into a poor baseline of health for some populations as they enter the second half of life.
THE SOCIAL CAPITAL OF OLDER ADULTS
Beyond SDOH, social connections are important drivers of health and well-being. The importance of social engagement to healthy longevity at both the individual and societal levels cannot be overstated. Figure 1-4 in Chapter 1 outlines the key enablers and disruptors of healthy longevity, and illustrates how social engagement can work with other enablers to influence a person’s health trajectory. People grow old within social networks of family members, friends, and others with a set of assumptions, expectations, and beliefs that shape their experience of aging. Societal perceptions of what it means to have a fulfilled, successful, or dignified life are diverse, and they change over time, but in all cultures,
social contexts, and countries, community institutions have a role in providing meaningful opportunities in which older adults can participate.
Social capital has been defined as “the connections among individuals, social networks and the norms of reciprocity and trustworthiness that arise from them” (Putnam, 2000, p. 19). The more recent literature suggests a new definition of social cohesion as “the ongoing process of developing well-being, sense of belonging, and voluntary social participation of the members of society, while developing communities that tolerate and promote a multiplicity of values and cultures, and granting at the same time equal rights and opportunities in society” (Fonseca et al., 2019, p. 246). The absence or decline of social cohesion can also be thought of as social erosion, with fewer citizens believing they are part of a moral community and having trust in one another (Larsen, 2014).
While a strong fabric of social cohesion provides many benefits to a community, one positive consequence is increased capacity for collective efficacy, with such outcomes as less conflict and violence in the community and increased formation of self-help enterprises, and a virtuous cycle from these benefits to improved bridging and bonding social capital. Social capital in communities has been found to have a “buffering” effect that counters the more adverse factors. For example, one study found that Hispanics and foreign-born citizens in the United States have a longer life expectancy than native-born non-Hispanics, which the authors attribute to strong social connections despite lower income levels (Singer et al., 2017). Social capital has also been noted as a key factor in resilience to and recovery from disasters. Following the Nepal earthquake in 2015, for example, researchers found that “high levels of bonding and bridging capital among residents reduced barriers to collective action” and assisted in rescue and recovery efforts (Panday et al., 2021). In the context of aging populations, the development of these connections across generations can be described as intergenerational cohesion, which can also have numerous advantages for families and societies. The United Nations recognizes intergenerational cohesion as essential to healthy societies (Butts et al., 2012).
Older adults have the capability to play a significant role in improving social cohesion both within and across generations, as well as increasing social capital, although opportunities to benefit from this capability have thus far been largely untapped. In the commission’s vision for healthy longevity (see Chapter 2), maintaining health into the second half of life will enable older people to remain engaged in their communities. With the right structures, older people could bring decades of accumulated knowledge and experience to the community and help younger people achieve success as they enter the workforce. Older people also provide care for grandchildren. The positive dimensions of aging and corresponding benefits to society can create social and human capital that can help address unmet needs and increase societal well-being (Fried, 2016). Social capital can be strategically and intentionally built, for example, by helping people who want to
work at later ages remain in the workforce and creating volunteer opportunities, as described in Chapter 3.
KEY TARGET: PROSOCIAL STRENGTHS OF OLDER PEOPLE
Being embedded in a larger social group holds powerful evolutionary advantages because humans are social beings. However, the nature of social networks changes with age. Abundant evidence demonstrates positive developmental trends in social and emotional functioning as people age, including evidence that older people are more prosocial than younger people. Prosocial behaviors are actions that benefit others (Cutler et al., 2021).
Quality relationships with families, kinship and friendship networks, and community ties, as well as the impact of social ties on health, remain important to well-being throughout the life course (Umberson et al., 2010). Evidence suggests that social networks narrow as people age (Lang and Carstensen, 2002). However, longitudinal findings suggest that the narrowing of social networks begins long before old age, which means it is not attributable to causes specific to aging (English and Carstensen, 2014). On the contrary, networks narrow selectively, such that people retain emotionally close social partners while eliminating more peripheral ones.
The current literature on social and emotional aging documents numerous positive trends in socioemotional functioning that contrast with stereotypes. Older people are more emotionally stable than their younger counterparts and often enjoy more positive emotional functioning in daily life (Carstensen and Chi, 2021; Carstensen et al., 2011). Notably, these emotional advantages were evident even during the COVID-19 pandemic, and studies validating this advantage of age during the pandemic have been replicated in scores of countries (Sun and Sauter, 2021). While aging is often associated with declines in cognitive function, a recent study found that social cognitive abilities and prosocial learning were more pronounced in older adults compared to those under age 36 (Cutler et al., 2021). Lack of concern for others was also found to be lower among older adults. Compared with younger and middle-aged people, moreover, older people experience fewer negative emotions in everyday life (Carstensen et al., 2011). They also express more gratitude, which in turn has been positively associated with physical and mental health (Emmons et al., 2003; Kubzansky et al., 2018). This evidence should inspire those in power to aim beyond simply addressing problems of vulnerable older people to work to build systems that leverage the social capital that increasing numbers of older and healthier people will bring to society.
Prevalent stereotypes of older people as regularly frail, burdensome, and dependent limit society’s ability to appreciate and capitalize on their potential human and social resources, which in turn undermines intergenerational cohesion and solidarity and threatens the achievement of inclusive, just societies
(WHO, 2020). Efforts to foster social connections and build cohesion start in local communities, where informal caring for family members, neighbors, and acquaintances is the norm.
Finding 4-2: Advancing age is associated with increased motivation to contribute to other people, younger generations, society, and the greater good. In addition, older people’s experience, knowledge, and emotional stability hold the potential to build the social and human capital needed to create and perpetuate healthy longevity.
Conclusion 4-2: Societies with healthy longevity can capitalize on the emotional stability and prosocial strengths of older people by enabling them in their existing roles and emerging new roles.
KEY TARGET: AGEISM AND AGE DISCRIMINATION
One of the most significant barriers to achieving healthy longevity is ageism. Ageism encompasses systemic stereotypes and prejudice, whether directed toward others or oneself—even many older people believe age-based stereotypes. Ageism can occur at the interpersonal level, between individuals; at the social level; or at the structural or institutional level (Marques et al., 2020). Because every person who lives to an advanced age will experience ageism, its scope and breadth are massive. In the European Social Survey, age discrimination was the most frequently reported form of discrimination for every age group. Among European countries, reports of unfair treatment of older people ranged from 17 percent (in Portugal and Cyprus) to 54 percent (in the Czech Republic), with an average of 35 percent (Ayalon, 2014). The COVID-19 pandemic has made ageist attitudes even more entrenched (see Appendix B). Structural ageism can also be found across sectors, including entertainment, marketing, social media, the workplace, and health care (Levy, 2022). Yet despite the scale of its negative impacts on older people and societies, “ageism remains a neglected global health issue” (Officer et al., 2020, p. 1).
Ageism is grounded in the belief that older people are fundamentally different from younger people. However, the old and the young actually have much in common; they work in the same jobs, maintain households, and participate in society. Media and advertising characterizations reinforce negative attitudes and biases toward older people. A 2019 AARP study found that adults over age 50 “represent only 15 percent of adults in online media images, and are seven times more likely to be portrayed negatively,” relative to younger adults (Dychtwald, 2021). Commonly held ageist attitudes are embodied in laws, policies, and institutions—particularly those related to health, social, and legal systems. When left unchecked, they can impede progress toward healthy longevity.
Older people experience the deleterious effects of ageism most directly. Once they are perceived as an “older adult,” they are exposed to external stereotyping and discrimination, as well as internalized ageist attitudes that are unconscious self-stereotypes. Worse health outcomes are seen among those exposed to ageism, including weaker and more negative social expectations of older generations, and internalization of ageist attitudes is “significantly associated with poorer physical and mental health in older adults” (Officer et al., 2020, p. 2). Accumulating evidence is also linking structural ageism to adverse health outcomes. According to a systematic review, 85 percent of 149 studies found that clinicians were less likely to offer treatments to older versus younger patients even if those treatments offered equal benefit regardless of age (Chang et al., 2020). At the same time, however, young people are not immune from discrimination. While more data are needed, attitudes toward younger people in Europe are more negative than attitudes toward older people (WHO, 2021a). Younger people are more likely than those in other age groups to report that they have been the victim of age-based discrimination. As evidence on cumulative exposures across the life course continues to demonstrate the importance of discrimination, it becomes clear that this is an area in need of greater attention.
In addition to its enormous burden in the area of health and well-being, ageism has substantial economic impact, costing countries billions of dollars annually (WHO, 2021a). One study found that negative age stereotypes, negative self-perceptions, and age discrimination in the United States led to estimated annual costs of USD63 billion for the top eight most expensive health conditions, and in Australia, estimates suggest the national economy would realize an additional AUD48 billion annually if 5 percent more people aged 55 or older were employed (WHO, 2021a). As discussed in Chapter 3, ageism is also a factor in decreased labor force participation among older people.
Compounded Discrimination
Ageism can interact with other forms of bias and exacerbate or compound the disadvantages they cause, greatly affecting an individual’s health and well-being (WHO, 2021a). A growing number of studies have explored the intersections between ageism and different forms of discrimination, including racism, sexism, ableism,2 heterosexism, classism, xenophobia, and others. Ageism and ableism, and ageism and sexism are two examples of multiple, compound, and intersectional discrimination that are especially pervasive.
Women constitute the majority of the older population around the world, but they often remain invisible to policy makers. Yet, they face unique ageism challenges that need to be accounted for in the global response to aging. In countries
___________________
2 Ableism is discrimination or prejudice against people with disabilities.
at all income levels, lifetimes of marginalization and discrimination, including unequal and inadequate access to education and jobs, compound the effects of ageism for women.
Women are more likely than men to engage in informal sectors of the economy and to perform unpaid work, such as caring for children and family members with disabilities and performing household work. Older African women, for example, contribute substantial amounts of unpaid domestic and care work, and often perform this type of work for longer relative to women in other regions/countries (He et al., 2020). In Latin America, for example,
[t]he overload of unpaid care work and the time-poverty that women face prevent equality of opportunity, rights, and outcome relative to men regarding participation in the labour market, but also social and political participation, and in the enjoyment of free time. Ultimately, the overload of this type of work on women limits their opportunities and stands in the way of their economic empowerment and also in the way of the possibility to enjoy their rights on an equal footing with men. (UN, 2020a, p. 7)
Although many older women contribute substantially to national economies, their lower rate of participation in the paid workforce across adulthood has cumulative negative consequences, including greater risk of poverty due to limited access to or low pensions (Bonnet et al., 2019). The caregiving burden often borne by women is exacerbated in such crisis situations as war, famine, forced migration, and epidemics or pandemics. Older women are negatively affected in these situations if they are not economically empowered because they rely heavily on the support of younger adults. To combat inequality, it will be essential to address the root causes and intersection of such prejudices as ageism and sexism. An example from Lebanon focuses on the engagement and empowerment of older women (see Box 4-1).
Interventions for Combating Ageism
A recent meta-analysis suggests that “relatively low-cost, feasible strategies involving education and intergenerational contact can serve as the basis of effective interventions to prevent ageism” and address the digital divide that keeps many older adults from using technology (Burnes et al., 2019, p. e1). In Australia, The Benevolent Society has conducted focus group discussions that have highlighted the importance of older people using their voice to combat ageism by participating in discussions regarding societal constructs of retirement ages and providing counter information and opportunities for other older people to reflect on their own internalized biases and ageism (Every Age Counts, 2017). In addition to educational campaigns, laws and policies can bring some needed strength to the importance of reducing and preventing age discrimination. As an example, the Organization of American States drafted the Inter-American Convention on the Protection of the Human Rights of Older Persons (OAS, 2017). It underscores that “older persons have the same human rights and freedoms as other persons,” which include the right not to be subjected to age-based discrimination or violence (OAS, 2017). Signatories agreed to accomplish this by adopting measures such as eradicating isolation, overcrowding, and food or medical treatment deprivation, and adopting or strengthening legislative or administrative measures to ensure adequate access to justice.
While some may assume that international frameworks such as the Universal Declaration of Human Rights (UN General Assembly, 1948) guarantee basic human rights to older people, ageism persists and is a violation of those rights. As is, the Declaration does not go far enough to address age discrimination against older people, and the rights of older people often remain invisible (Mokhiber,
2018). Even documents such as the Madrid Plan of Action are not legally binding and ask governments for commitments, so many are calling for a UN Convention on the Rights of Older People to combat ageism, clarify responsibilities, improve accountability, and guide policy making (UN, 2010).
Recognition of ageism as an SDOH could also help eliminate it (WHO, 2020). For example, WHO Africa and HelpAge International have organized a regional campaign to raise awareness of the magnitude and impact of ageism. The main objective is to strengthen the capacity of African countries by sharing resources and tools to establish a community of young advocates who work to change the narrative around aging (WHO Africa, 2021). Interventions that include both education and intergenerational contact demonstrate especially strong effects, especially for combating negative attitudes toward and perceptions of aging (see Box 4-2).
Levers for Empowering Change
Overcoming ageism will require societies and individuals to change the way they think, feel, and act toward age and aging (WHO, 2021a). It will also require dual approaches to reducing and preventing further ageism at both the individual and structural levels. Educational efforts can help more people see the value of older adults and change stereotypes, but different solutions will be required to change the more structural biases embedded in institutions such as health care and the workplace. Addressing this key target is a complex and multifaceted challenge that will require long-term attention. But the actions called for in this report align with other expert reports calling attention to similar needs and approaches. For example, the WHO Decade of Healthy Ageing (2020) report also emphasizes the need to change how people think and feel about aging (reducing ageism), calling on member states to adopt legislation banning age-based discrimination and supporting the development of programs to reduce and eliminate ageism in several sectors.
Finding 4-3: Ageism is a barrier to achieving healthy longevity across all countries and cultures, especially when compounded with other forms of discrimination, such as sexism or racism.
Finding 4-4: Countries have initiated successful programs to combat ageism by creating a culture with positive expectations of and about older people to improve the well-being and productivity of people as they age.
Conclusion 4-3: Greater attention to the prevalence and pervasiveness of ageism in all sectors is warranted. Combating ageism will require
a range of responses, from eliminating ageist laws, regulations, and policies; to ending discrimination based on age; to modifying cultural attitudes about older people’s capacities. Public information campaigns can promote the value of older people and attack stereotypes, while advocacy efforts can bring generations together to fight discrimination and recognize ageism as an essential element of efforts directed at diversity, equity, and inclusion.
Recommendation 4-1: Governments should develop evidence-based, multipronged strategies for reducing ageism against any age group by
- collaborating across sectors—for example with local governments, industry, and nongovernmental organizations (NGOs)—to launch public information campaigns that highlight the value of older people to society;
- developing public and private partnerships to create programs, connected intergenerational communities, and innovative models that enable all people to contribute to society; and
- developing legal protections for the rights of older people and ending age-based segregation and discrimination (e.g., legal barriers related to housing, policies that discourage work at older ages).
Metrics
While there must be a careful balance between prioritizing existing and validated metrics and being open to different ideas in evaluating policies and programs based on a range of outcomes, there is utility in tracking indicators related to the reduction of ageism. The WHO Decade of Healthy Ageing (2020) report also highlights indicators related to the SDGs but modified to track the progress of older adults specifically. For example, specific to this key target of combating ageism, WHO recommends (WHO, 2020)
- Indicator 10.3.1: Proportion of population who reported personal discrimination or harassment in the previous 12 months on the basis of grounds of discrimination (age) that are prohibited under international human rights law.
Research Questions
While many recommendations and metrics have been released in recent years as this topic has grown in importance, many interventions still lack solid evidence, and questions remain about how best to prioritize resources and populations. Following a literature review conducted in the United Kingdom, researchers at the University of Birmingham noted the paucity of research on how aging is experienced by different cultural groups (Field and Fenton, 2014).
Because data are limited, WHO suggests the need for research “producing estimates of the economic impacts of ageism and determining how ageism contributes to poverty among older people, its wider costs to national economies, and how ageism contributes to slowing social and economic development, particularly in low- and middle-income countries” (WHO, 2021a, p. 57). Additionally, the effectiveness of laws and regulations in addressing ageism has been demonstrated, but there is a need to expand the evidence base in low- and middle-income countries, and more robust systematic reviews are needed to determine the strength of various interventions (WHO, 2021a). While intergenerational cohesion is discussed further in the next section, there is a need for “research to determine the optimal conditions under which contact between grandparents and grandchildren and intergenerational friendships lead to reductions in ageism” and “development and testing of interventions to foster these relationships and reduce ageism” (WHO, 2021a, p. 134). Finally, knowledge is insufficient on the scale and impact of ageism directed at younger populations. Although this report focuses mainly on older adults, given the high proportion of young people in many countries and extended life expectancies, understanding these interactions and potential discrimination that occurs between generations is another opportunity for greater insight.
KEY TARGET: SOCIAL INCLUSION
Isolation is defined as the experience of being alone (a state of objective physical separation), while loneliness refers to perceived isolation and lack of satisfying emotional connections to others. Humans are not meant to survive alone. The perception of isolation and feelings of loneliness have negative consequences for socioemotional and physical health and are risk factors for disease and early death (NASEM, 2020). Loneliness is often associated with old age but has been increasing in people of all ages in recent decades. Research has found that loneliness levels actually peak before the age of 30, then diminish through middle adulthood into early stages of old age. After a person turns 80, reported loneliness begins to increase again, to levels comparable to those of younger people (Luhmann and Hawkley, 2016). Thus, while it is wrong to assume that older people as a group are lonely, a significant minority do report loneliness. The challenge is worldwide, with an estimated 20–34 percent of older adults in China, Europe, Latin America, and the United States identifying themselves as being lonely (WHO, 2021b).
Aside from emotional impacts, loneliness is associated with poor health outcomes including depression, dementia, heart disease, and other conditions (Singer, 2018). The combined neurobiological effects of loneliness on sleep, executive functioning, and mental and physical well-being contribute to higher rates of morbidity and mortality in older adults (Cacioppo and Hawkley, 2014). The costs of social isolation and loneliness are only beginning to be fully appreciated. In the United States, for example, social isolation adds an estimated USD6.7 bil-
lion to Medicare spending annually (Flowers et al., 2017). In many high-income countries experiencing historically low birth rates and longer lives, increasing numbers of older people are living alone without other family members, raising concern that loneliness may be more prevalent in the future.
Cultural and social factors across the life span can affect a person’s ability to achieve healthy longevity. As discussed earlier in this chapter, social capital and social cohesion can be particularly influential toward building strong communities and keeping adults engaged as they age. But ongoing demographic changes will require greater attention to minimizing age segregation and ensuring ongoing social connection, which can help combat loneliness. Some potential mechanisms to this end include leveraging religious and spiritual connections, empowering older adults within communities, and creating opportunities for intergenerational connections and cohesion. Societies can support these and other intergenerational programs to promote healthy longevity.
Finding 4-5: Older people have lower rates of loneliness relative to younger people, but rates begin to rise again after age 80. When paired with the increasing prevalence of chronic conditions as people age, this rise in loneliness can contribute to several comorbidities affecting healthy longevity.
Leveraging Religious and Spiritual Connections
Healthy aging is positively associated with religiosity and spirituality. As people age, they can be more likely to consider spiritual questions with greater importance to and influence on their lives. There is evidence of positive correlations “between self-forgiveness, spiritually motivated forgiveness, and psychosocial well-being” (Banerjee, 2021, p. 66). While spirituality can be an abstract concept, there are numerous practical manifestations, such as gratitude, meditation, forgiveness, sense of purpose, and volunteering (Banerjee, 2021). There are also benefits to a formal religious community. Focus groups in the United Kingdom, for example, identified as a theme the sense of community and belonging gained through participating together and related social activities such as sharing meals (Malone and Dadswell, 2018). Drawing on these roles and understanding the importance of religion and spirituality in the lives of older adults can help inform the discourse on healthy longevity.
Identifying these connections can also provide linkages across generations and help promote healthy longevity across the life course. A systematic review examined the effect of spirituality and religiousness as a predictor of quality of life for young people and overwhelmingly found positive associations (Borges et al., 2021). The most predictive factor for good quality of life was the spirituality the participants adopted—components such as hope, optimism, inner peace, and faith—even without a formal religious affiliation. Researchers also found positive effects on mental health. Across studies, positive influences of religion
and spirituality on quality of life and healthy longevity were noted, despite the heterogeneity in how people come together to worship and what the various settings look like.
Empowering Communities and Engaging Older Voices
Fostering social inclusion in communities requires creativity when government resources are stretched and populations are aging rapidly. Overall, fostering community advocacy and seeking the voice of older people are valuable policy goals that could complement the more traditional roles of advocacy for prevention of abuse of older people (Field and Fenton, 2014). Biological age cutoffs are not useful markers for understanding the needs of older people, and having a more nuanced understanding of aging across the life course would provide additional insight. One approach to engaging older people is through participatory design, ideally to bring underrepresented groups and minorities into the decision-making process that directly affects them, which differs from the traditional top-down decision-making model. A study in New Zealand with the Maori community summarizes steps in that community’s approach as “(1) understanding of place, (2) relationship building, (3) respectful facilitation, and (4) empowered participation” (Marques et al., 2018, p. 6). Using a collaborative approach in seeking feedback and informing the design of programs and policies can result in greater sustainability and social benefits because the results acknowledge that different people can experience different realities.
Without an opportunity for the voices of older adults to be heard and incorporated into community and urban development, it will be impossible to truly meet their needs and optimize the environment for healthy aging across the life course. Engaging people in their own community development is more important than ever today, given the rate of population aging and the availability of older adults as an underutilized resource (HelpAge International, 2016b). Community-level interventions are effective and can lead to improved earning, healthier residents, and more active participants in the community. In Taketoyo, Japan, for example, the implementation of community-based centers, or “salons,” where senior residents could gather showed a protective association against cognitive decline among those over 65 who participated (Hikichi et al., 2017).
Each region and country will have its own methods for incorporating the voices of older adults, but the Older People’s Associations (OPAs) found throughout Asia are a good example. A four-country study conducted in 2017 found that OPAs can make a true difference in the lives of older people, and can be used to develop local structures to fill the gaps between families in need of assistance and governments with limited resources (Howse, 2017). Keys to success for an OPA include strong management, sustained funding, and active and engaged members (HelpAge International, 2016b). Box 4-3 highlights a pilot project in Vietnam that promotes healthy longevity through a variety of community-driven activities and interventions.
Intergenerational Cohesion
Globally, economic security, social norms, and cultural values form ties within communities composed of families, kinship groups, and nonfamilial groups. When these ties are robust, with opportunities for interaction among different subpopulations, such as intergenerational social networks, cohesion is strong, and loneliness is less likely. Intergenerational social networks differ among countries and regions, but the dominant norms emphasize the importance of intergenerational connections and the protection they can provide against social isolation and loneliness. Importantly, benefits are seen across generations, not just among older adults.
Intergenerational programs have been developed by the public and private sectors. Although their effectiveness and optimal parameters are still being refined, benefits are widely reported for such programs. Older adults in these programs become less isolated and feel less lonely, and experience improved health
and well-being (Jayson, 2018). Older adults with dementia experience positive effects and increased engagement when interacting with children when compared to activities that do not mix generations. Benefits accrue to the children in these programs as well, including improved learning and social development and more positive perceptions of older adults (United for All Ages, 2018). To generate these benefits, some organizations have created intergenerational play programs or classrooms designed to bring disparate age groups together. In the United States, for example, the St. Ann Center in Wisconsin specializes in adult and child day care services that include an intergenerational activity or class twice a day that provides an opportunity for the groups to interact and learn from one another (St. Ann Center, 2021). A systematic review of intergenerational programs examining benefits for children and older adults found improvements in attitude, behavior, confidence, and competence for the children, along with “significant differences in mental and physical health and quality of life for the older adults” (Giraudeau and Bailly, 2019, p. 363). However, the design and implementation of these programs is key to their success, and benefits will not be automatic.
Another approach to building intergenerational connection is illustrated by the Cycling Without Age program, started in Denmark in 2012 (Cycling Without Age, 2021). Limited mobility was preventing older adults from riding bicycles, so the program obtained “trishaws” that seat two people in front and the cyclist (usually a younger person) behind. The program gives older people an opportunity to remain an active part of society and the local community while also creating new relationships between generations. Younger people volunteer to drive the older riders and have the opportunity to hear stories from them before those stories are forgotten. The program currently has 2,700 chapters in 52 countries.
Another mechanism for building or maintaining strong connections across generations, directly and indirectly, is through multigenerational households that pair either older and younger generations or families. An increasing number of innovative examples of such arrangements have emerged worldwide as housing has become a shrinking, desirable commodity and older adults strive to age in place. Critical evaluations of these arrangements are often lacking, and because of variability in cultures and contexts, what works in some places may not work in others. Nonetheless, drawing lessons from successful interventions involving multigenerational households can guide the future development of such programs. In the Netherlands, for example, experiments in which college students live with older people began in 2012. This quite successful housing scheme, often dubbed “free rent for companionship,” provides students free housing in exchange for 30 hours per month of their time spent with their older housemates (The Economist, 2019a). Similarly, a study in France found that intergenerational housing arrangements solved two pervasive problems in the city of Paris: caring for older adults and providing affordable housing (Holman, 2019). 61 percent of people aged 18–30 living in one of these arrangements said they would not have had access to traditional housing otherwise, and more than half of the older
adults reported that having a young person living with them allowed them to delay moving into a retirement home.
Adults of all ages are at risk of social isolation and shrinking family ties as a result of global trends toward smaller families and employment-related migration (Cacioppo and Hawkley, 2003). While families have varying reasons for multigenerational living, they often go beyond a desire for connection, reflecting structural pressures and individual circumstances, such as affordability, divorce, or illness, that make these arrangements the most practical option (Burgess and Muir, 2020). Among rural dwellers in Myanmar, for example, close proximity or coresidence of older people and their adult children’s families provides personal material support and services (Knodel and Teerawichitchainan, 2017). Multigenerational living offers other benefits aside from potential financial savings. In one study, healthy subjects in the United States who lived in two-generation housing had lower premature mortality than those who did not (Muennig et al., 2018). And researchers in China found that men and women who lived in an institution or moved to such a facility after living with family faced a greater risk of dying relative to those who continued living with family (Feng et al., 2017).
Living arrangements are highly variable depending on culture and region. In North America and Europe, one in five older adults live alone (UN, 2019a), while in Asia, Africa, and Latin America and the Caribbean, more than 75 percent of older people live with children or extended family (Kamiya and Hertog, 2020). Evidence suggests, however, that these numbers may be shifting. A recent study found that multigenerational living is on the rise in the United States: one in four Americans now live in a household with three or more generations, representing a four-fold increase in multigenerational households in the past decade (Generations United, 2021). Box 4-4 describes a variety of influences and factors that may be at work in shaping intergenerational households in different countries.
Levers for Empowering Change
Lack of social inclusion can impede healthy longevity. Efforts to address loneliness and intergenerational cohesion can help promote social inclusion in communities and serve as entry points for addressing other needs, including housing, food, and transportation. Cities and communities are increasingly creating programs to connect people across generational gaps, recognizing the benefits for all participants. Given the high levels of loneliness reported by younger adults, bringing age groups together can yield benefits for both older and younger people. Research and evaluation of existing programs will be needed to develop a clear understanding of the best such interventions in specific contexts. Countries and communities will need to monitor the effects of changing dynamics as younger families opt to live separately from older generations or move to other parts of the country for work. In the face of such changes, it will be important to maintain, encourage, and support social roles for older adults.
Finding 4-6: Intergenerational programs globally provide diverse opportunities to address loneliness at all ages, with the potential to achieve improvements in other targets, such as reducing ageism.
Finding 4-7: While intergenerational living offers several benefits, different countries and contexts may see the makeup of households shifting
with demographic change, creating the risk that more older adults will be living alone in some areas.
Conclusion 4-4: Generating increased social inclusion in communities will require a multidisciplinary and layered approach combining strategies from various sectors. Targeted efforts are needed to strengthen social networks and reduce loneliness, especially in places where demographic shifts are leading to smaller families and family separation.
Metrics
Similar to this report’s findings and calls to action, the WHO Decade of Health Ageing (2020) report advocates for ensuring that communities tap the abilities of older people and foster intergenerational cohesion, calling for the inclusion of older adult voices and stimulation of intergenerational dialogue. Related to fostering social inclusion, the WHO report suggests the following metric to gauge progress:
- Indicator 5.4.1: Proportion of time spent in unpaid domestic and care work, by sex, age and location, as a basis for provision of public services, infrastructure, and social protection policies.
In addition to the SDG indicators, some countries now capture and publish measures of well-being, which are aligned with the SDOH in the WHO list. For example, the United Kingdom has created a dashboard to track “Measures of National Well-Being” to support its national program, and monitors the personal well-being, relationships, health, work, leisure activities, and living situations of citizens, among other indicators (UK Office for National Statistics, 2019).
Additionally, the Active Ageing Index is a tool that can measure the untapped potential of older people for active and healthy aging (UNECE/European Commission, 2018), providing a mechanism to guide public policies. Relevant to the key target of social inclusion, the index measures
- the number of older adults who provide care for children, grandchildren, or older adults;
- the number of older adults who live independently;
- relative median income and those with no poverty risk;
- mental well-being; and
- level of social connectedness (measuring contacts outside the household occurring by choice).
However, the Active Ageing Index has been tested only in Europe, and other countries may require a broader set of metrics for evaluating their environments
for aging. The Scaling Healthy ageing, Inclusive environments, and Financial security Today (SHIFT) Index (The Economist, 2019b) benchmarks each G20 country’s performance using 59 subindicators. Categories related to this chapter include the following, with additional detail on methodology found in the above-referenced article in The Economist:
- Indicator 1.3: availability of health and social care services;
- Indicator 3.1: social cohesion and participation; and
- Indicator 3.4: presence of inclusive social institutions.
Research Questions
More research is needed to identify the best intergenerational policies and programs and inform the creation of new policies and programs. The development of intergenerational programs has been increasing around the world to build social cohesion and bring benefits to multiple age groups, but how best to design such programs for successful implementation and optimized effects remains unclear. More monitoring and evaluation of these programs, especially to understand the return on investment, can provide important insights for communities looking to enhance their social inclusion and reduce loneliness among their residents.
As the proportion of older adults continues to grow, another question that could illuminate life-course trajectories in many low- and middle-income countries is the underappreciated role of young caregivers, especially for older family members. A systematic review has highlighted the positive and negative impacts on young people’s everyday life, but more studies are needed to better understand different aspects of caregiving and design appropriately tailored services (D’Amen et al., 2021). There also are unknown societal costs of having young people forego their education to care for dependent older adults, costs that in Mexico, for example, have been estimated to be high (Gutiérrez-Robledo et al., 2021).
KEY TARGET: FINANCIAL SECURITY IN RETIREMENT
Comprehensive financial security systems are critical to mitigating socioeconomic inequalities and providing opportunities for individuals and families to navigate their health, education, and work circumstances to contribute to society. Financial security is an ageless need. Regardless of work history, gender, disability, or position in society, all people require a reliable, adequate income over the life course. Financial security benefits everyone because people with a secure income can contribute to their communities, have good quality of life, and live with dignity. But the right systems, structures, and opportunities must be in place for population-wide financial security to become a reality. The collection
of these systems, structures, and opportunities can look different across regions and countries, but includes at a minimum pensions and social protection against poverty, vulnerability, and social exclusion; work that provides a fair income, safe working conditions, and equal opportunities; and access to financial services without discrimination (HelpAge International, 2021).
In many parts of the world, national and local governments are responsible for delivering on positive outcomes for the social enablers of healthy aging since they have the infrastructure and capacity to make change within and across generations. While high-income countries have established financial security systems, many low- and middle-income countries do not yet have such old-age protection for all of their population. Most countries offer old-age pensions to formal-sector employees only, leaving those in the informal work sector exposed to financial insecurity. Even in high-income countries, however, social security systems were instituted before population aging became an issue. Consequently, existing financial security systems were often designed for shorter lives and so lack mechanisms for adjusting the retirement age to reflect demographic change. Adjusting the retirement age is politically contentious in most high-income countries, but failure to do so can result in financial crisis, delayed disbursement, and reduced social pensions, affecting the most vulnerable older people who depend on social security for a living. Globally, this challenge can be an opportunity for those nations with less well-developed systems to design a better system from the ground up and learn from past lessons of other countries that will need to redesign their financial security infrastructure to be a more appropriate fit for the future.
Financial security schemes are an example of equitable income access and transformation of opportunity structures within communities, supporting the most vulnerable people in society. As described previously, poverty can have a critical influence on life expectancy, and differences of just a few miles within a city can translate into several years added to or subtracted from a person’s life. A few countries (e.g., Australia, Denmark, the Netherlands, Switzerland) have successfully implemented systems that include generous health-promoting social structures, usually, although not always, means-tested, to meet the objective of alleviating poverty. They also have mandatory private saving plans, sometimes called “prefunded” plans, to help achieve consumption smoothing—essentially, the tendency of individuals to alter their spending and saving habits throughout their life depending on available resources. These designs are much more sustainable than others, as indicated by a global pension index that routinely places the systems of these countries near the top of its rankings for their sustainability (Mercer, 2021). Still, striking differences are evident across regions and countries with regard to pension availability and the structural and sociocultural contexts in which they were created. For example, only 12 African countries have established national pension schemes, and only 5 of those are universal (He et al., 2020). Furthermore, it is estimated that worldwide, more than 95 percent of
people above retirement age in Europe receive a pension, while this is the case for only 26 percent in Central and Southern Asia and 23 percent in sub-Saharan Africa (UN, 2018).
Finding 4-8: Regardless of their work history or social status, financial security into older age can allow people to live with dignity, contribute to their communities, and have good quality of life, especially when they are unable to work. Absent this security, lack of access to necessary resources can have a detrimental effect on people’s health and life span.
Testing Different Social Protection Models
Projections of increasing life expectancy across countries and the continued disparities among racial and socioeconomic groups help make the case for a widespread commitment to financial security for older people, although different cultures and communities may need to customize their financial security schemes to fit their populations’ unique needs. A series of papers demonstrates that means-tested social pensions are advantageous in economic welfare terms compared with alternative formulations (Kudrna, 2017). The alternative formulations examined employ contributions-based and earnings-related social security, as in the United States, or a universal, flat-rate, noncontributory social pension.
Several mechanisms explain the benefits of a means-tested social pension. First, the lower revenue requirement with means testing reduces the tax increases needed to finance the pension scheme. Additionally, higher-income households have the most discretion over their saving and labor supply, so means testing avoids the potential adverse incentive impacts of a universal pension. Finally, a social pension with a single access age operates regressively in the absence of a means test but progressively with a means test. Costs of administering a means test have been found to be much lower than those of tracking contributions for social security entitlements (Baker and Rho, 2011). The report of the Commission on Funding of Care and Support in the United Kingdom recommended continued means-tested support for those of lower means, noting that not everyone will be able to afford to make personal contributions (Commission on Funding of Care and Support, 2011). However, the commission recommended that those who enter adulthood and already have a need for care and support should be immediately eligible for state support without further inquiry.
Conversely, implementing these policies in countries with entrenched social security systems based on contributions from the formal workforce is politically very challenging. In emerging economies where most of the labor force operates informally, creating a new social protection system for all is more feasible. A lifetime of SDOH factors influences people’s circumstances at older ages; those who have faced adverse consequences from SDOH across the life span are more
likely to have functional challenges that impact their ability to work and provide for themselves at older ages. A basic social pension allows people to exit the workforce—formal or informal—and still have the financial support needed to survive. Even if countries can start with a baseline minimal amount, these initial efforts can validate the concept and lead to incremental changes. The key is to structure and create policies and institutions that promote people’s intrinsic societal value irrespective of age, ability, or choice to engage in paid or unpaid work. This basic precept aligns with the International Labour Organization’s (ILO’s) recommendation for national standards of social protection and “guidelines for implementing and monitoring national strategies that are participatory, country-led, sustainable, and regularly reviewed” (UN, 2013, p. 6). ILO also provides guidance to member states on progressively providing additional protection to as many individuals as quickly as possible, in accordance with a country’s economic and fiscal capacities (Cichon, 2013).
Interventions to Ensure Financial Security
Many countries have tried various interventions to improve the financial security of their residents. These interventions range in breadth and depth depending on the country’s needs and circumstances. In 2015, for example, Australia reformed its welfare system, which led to an investment approach that ensures that funds are invested in groups of people with the largest anticipated future lifetime costs and the capacity to transition to self-reliance. The approach was established as part of the country’s 2015–2016 national budget, with funding totaling AUD66 million (Australian Government, 2015). A different approach was taken by Brazil at the turn of the 21st century, when it was facing high levels of hunger, poverty, and inequality in many of its densely populated cities. The government introduced the Programa Bolsa Família in 2003 to provide conditional cash transfers for low-income families to ensure that their children could attend school and receive childhood vaccinations. Years later, the program’s results demonstrate that it has reduced the proportion of the country’s population living below the international poverty line from 13 percent to 3 percent. Bolsa Família is also credited with 12–21 percent of the country’s reduction in income inequality and is widely seen as a model for conditional cash transfer programs (Centre for Public Impact, 2019). While this program is focused on families and young children, the long-term effects of providing these levels of security for younger adults will be influential in their aging trajectory, improving their chances of healthy longevity.
Addressing the wealth of workers in the informal sector can present an added challenge for many low- and middle-income countries. The size of the informal economy as a share of GDP in Africa is the largest in the world (Guven et al., 2021). Understanding this group will be key to successfully expanding social
protection schemes, which will likely include instruments such as safety nets, economic inclusion programs, and productivity-enhancing measures—as outlined in the World Bank’s report Social Protection for the Informal Economy (Guven et al., 2021). In Togo, for example, more than 92 percent of the workforce is considered informal (WIEGO, 2022). After years of stalled progress in including these workers in social protection programs, a combination of a top-down and bottom-up approach bringing together international organizations such as ILO and civil society advocacy groups led to better understanding on the part of the government and greater awareness among informal workers. As additional case examples, Box 4-5 highlights the design and outcomes of three recent social protection programs in low- and middle-income countries that have seen success.
Levers for Empowering Change
Effective national social protection systems help build inclusive societies and reinforce “social cohesion by protecting individuals from social risk” and economic deprivation (UN, 2013, p. 4). Financial security systems are “a powerful instrument for providing income security and reducing poverty and inequality,” and also play a role in ensuring older people’s access to basic needs, such as health care, housing, education, and food (UN, 2013, p. 4). Yet, actionable policies to prevent the detrimental effects of poverty and inequality on health have still not benefited the most disadvantaged. If people have no income security or resources once they can no longer work, their chances of achieving healthy longevity decline significantly. Ideally, financial security systems would guarantee that all vulnerable people (not just older people) have a secure income from social insurance or a tax-funded minimum social pension to prevent them from falling into poverty, alleviate their financial dependence on family members (and thus reduce the risk of wider poverty), and ensure their financial autonomy and dignity. However, this vision will not come without challenges, as along with the increasing inequality within countries over the past decades, governments have faced decreasing resources. The World Inequality Report of 2020 notes that countries have become richer over the past 40 years, but the share of wealth held by public actors is close to zero, with the overwhelming share in private hands (Chancel et al., 2022). The low level of government wealth will make it difficult to implement social pension programs for a greater share of aging citizens.
The commission observes that countries will require different types of programs to improve financial security for older adults as appropriate for their populations and cultures. While recommendations similar to those in this report have been made before, they have not always been implemented. Different countries may internalize different perceptions of need, making decisions to prioritize other sectors with their limited resources. These are difficult decisions, sometimes based on incomplete or outdated information given changing populations, economic variability, and the increasing inequality within countries. Some countries, such as those featured in Box 4-5, have decided that the risks associated with protecting more of their population come with important benefits for their population’s longevity, even if those benefits are realized only over the long term and only through iterative program designs. Regardless of the approach a country takes, greater knowledge and awareness among the public of the importance of financial security in older ages will be required. The Commission on Funding of Care and Support in the United Kingdom, for example, has recommended an awareness campaign on the importance of planning ahead, as well as robust information and advice strategies for the public so people can access reliable information on available services and funding sources (Commission on Funding of Care and Support, 2011).
Finding 4-9: The identification of eligible residents and payment of benefits to people in isolated communities have become feasible and reliable.
Finding 4-10: Financial security is an enabler of healthy longevity. Social pensions offer an effective way of delivering financial security for older populations and will become more prevalent as the demographic transition continues.
Conclusion 4-5: Financial safety nets for older people are essential to achieving healthy longevity, especially in low- and middle-income countries, where informal labor force participation is high. Regardless of work type, all people need to be covered by pension and social protection programs. Additionally, support for individual retirement savings will require that people have financial literacy and universal access to secure banking systems and investment opportunities.
Recommendation 4-2: By 2027, all governments should develop plans for ensuring basic financial security for older people.
- For countries without retirement income systems, introduce support for older people with no or subsistence-level income.
- For countries with emerging retirement income systems, increase security for low-income older people.
- For countries with robust retirement income systems, identify evidence-based models for strengthening financial security across the life course.
Recommendation 4-3: To improve financial security in retirement, governments and employers should develop strategies for increasing financial literacy and mechanisms for promoting pension contributions, self-funded pensions, and lifelong savings.
Metrics
Other reports have advocated for greater financial security and income protection for citizens. The WHO Decade of Healthy Ageing (2020) report, for example, calls for support for income security across the life course. Additionally, the SHIFT Index (The Economist, 2019b) uses the existence of national pension systems as a metric for its scoring. And some SDG progress indicators align with the goals and targets discussed in this chapter, including the following (UN, 2021):
- Target 1.3: Implement nationally appropriate social protection systems and measures for all, including floors, and by 2030 achieve substantial coverage of the poor and vulnerable.
- Indicator 1.3.1: Proportion of population covered by social protection floors/systems, by sex, distinguishing children, unemployed persons, older persons, persons with disabilities, pregnant women, newborns, work-injury victims, and the poor and the vulnerable.
Research Questions
Further research can guide new policies and programs to provide social protection for aging populations. Greater insight is needed in many areas. One area is the impacts of such policies on labor force participation and health status of older people, and the interaction between the two. As older adults seek to leave the workforce and maintain their wealth, research also is needed on alternative approaches for generating engagement in financial competence and knowledge. Financial literacy is one important focus; others include incentives to save for the long term, the long-term impacts of default design for saving, mandatory saving, and the links between life-course health patterns and financial security, all of which need more research.
KEY TARGET: DIGITAL LITERACY
Another contributor to the challenges of aging is the lack of digital literacy among older adults, whereby those who are unfamiliar with computers and new devices are increasingly being left behind as technology advances and becomes ubiquitous in daily life. This has led to the “digital divide.” Physical access to broadband technology, discussed in Chapter 5, is one key component of addressing the digital divide. This section focuses on the social aspects and root causes of the lack of digital literacy and how it can be used to achieve healthy longevity.
Older adults continue to be the least likely age cohort to have access to the internet because of both physical and psychological factors (Chu et al., 2021). According to a European Union report, one-third of older adults reported never using the internet (Anderson and Perrin, 2017). This issue has been percolating below the surface for years, but the onset of the COVID-19 pandemic has amplified its importance. In China, for example, news reports highlighted an older woman who wanted to pay for her medical insurance in cash but was refused because of contamination concerns. Because she did not have mobile payment capability, she was left without options. Similarly, an older man in China was refused bus access because he did not have the mobile app to show his health status code (Kidron and Yang, 2021).
Reasons for this lack of digital literacy are numerous. One study in South Korea examining people over age 55 found digital engagement to be significantly influenced by factors such as gender, academic background, usage motive, life satisfaction, and household type (Yim et al., 2020). Interestingly, in Singapore, poor health has been found to be a main cause of the digital divide among older
people, as health problems can affect a person’s online communication and social activities within their networks (Ang et al., 2021). In Latin America, many older people live in homes with internet access, but they do not use the internet, highlighting barriers such as lack of motivation or desire (Sunkel and Ullmann, 2019). Given that there is no single reason for the lower levels of computer and internet use among older adults, solutions for increasing digital engagement across this population will be multifaceted.
Recently, a Lancet and Financial Times Commission stated that weak governance of digital technologies contributes to inequities and compromises human rights (The Lancet and Financial Times Commission, 2021). While much of that commission’s focus is on youth, especially in low- and middle-income countries, interventions beginning with young people and continuing across the life course can have important implications as people age. Those who are educated in and immersed in digital technologies from a young age will likely continue to use technology throughout their lives. The Lancet and Financial Times Commission argues that digital access is a determinant of health, and technology needs to become a positive driver for equity. Otherwise, existing inequities will be exacerbated by the widening digital divide.
A WHO report addresses “the potential interplay between ageism and AI [artificial intelligence] for health as it affects older people, including the conditions in which AI for health can exacerbate forms of ageism and whether use of AI for health introduces new forms (or risks) of ageism” (WHO, 2022a, p. 3). The report emphasizes that “[l]egal, nonlegal, and technical measures can be used to minimize the risk of ageism in AI and to maximize its use for older people as these technologies become more widespread” (WHO, 2022a, p. 2). As AI technologies revolutionize aspects of public health and medicine and can be especially important for older people who have several comorbidities or conditions to monitor, the technologies can lead to harm without careful and ethical oversight. Indeed, numerous studies have highlighted the potential for embedding biases in AI systems as they rapidly develop (Chu et al., 2021). A WHO policy brief on Ageism in Artificial Intelligence for Health notes that the datasets used to train AI models and improve machine learning often exclude older people. Additionally, it is rare for design teams building these models to include older people; instead, they overwhelmingly include young White men. This increases the likelihood that older people will be excluded from new AI technology and that technologies targeting them will be inappropriate. Remedies for this challenge include leveraging participatory design approaches for AI technologies to involve older people, and having age-inclusive data collection and age-diverse data science teams (WHO, 2022a).
Interventions to Improve Digital Literacy
As with many interventions, implementation focused on digital literacy will have multiple positive effects across policy needs for different groups. Lifelong
learning opportunities and affordable, accessible “smart” digital cities and rural and remote communities can help ensure that the needs and abilities of older people and those with disabilities are addressed. As these interventions proliferate, however, the importance of equity in opportunities will remain central.
Improving digital inclusion among older adults will require increased access to and motivation to use the internet and computers and digital skills. To address these various factors, countries in Latin America have implemented programs to promote digital inclusion among older people. For example, a pilot program was launched in Uruguay in 2015 to advance equal access to knowledge and social inclusion among retirees (Sunkel and Ullmann, 2019). Targeting low-income older adults, 100,000 electronic tablets designed for older adults were provided during a workshop in which participants were taught how to use the technology and relevant apps. Keeping in mind multigenerational and life-course concerns, the program also included a campaign to help children and grandchildren of the beneficiaries use the technology.
Levers for Empowering Change
To improve digital inclusion, a Brookings report by Tomer and colleagues (2020) emphasized the need to engage trusted actors and institutions from the private and public sectors when evaluating needs and developing interventions for specific populations, such as communities of color and immigrants. Primary schools, public libraries, and other nonprofit organizations are potential providers of digital literacy interventions. Additional targeted efforts to understand what digital skills are necessary for work and how to build those skills are also needed.
Increasing older people’s access to and familiarity and comfort with digital technologies have the potential to decrease isolation, increase engagement, and improve access to virtual services such as telemedicine, as seen during the COVID-19 pandemic (Haase et al., 2021). Access is inhibited, however, by ageist myths that older people are rigid in their thinking or unable to understand and use emerging digital tools. Investing in digital infrastructure designed for older people and incorporating age-diverse representation in AI and machine learning algorithms could help to close the digital divide.
Finding 4-11: Education to increase digital literacy among older people can help them to integrate into societies with rapidly changing technological advances and provide them with increased opportunities for engagement.
Conclusion 4-6: As technology rapidly advances, targeted digital literacy efforts, paired with participatory design for AI technologies to involve older adults and age-diverse data science teams, are needed to enable older adults’ full participation in society.
Metrics
Also relevant to the need to narrow the digital divide and improve digital literacy among older adults, the WHO Decade of Healthy Ageing (2020) report highlights indicators related to the SDGs but modified to track the progress of older adults specifically:
- Indicator 4.4.1: Proportion of young people and adults skilled in information and communications technology, by type of skill, also distinguished by older people; and
- Indicator 17.8.1: Proportion of individuals using the internet (disaggregated by age).
Research Questions
While there is a wealth of research on the benefits of volunteering for both physical and mental health (see Chapter 3), the potential for older adult volunteers to act as ambassadors to other older adults to promote digital literacy represents a research opportunity. Calls from the United Nations to collaborate across the public and private sectors to create more user-friendly technologies and engage older people in digital societies note the need for shared understanding of older people’s values and abilities to cocreate digital environments (UN, 2019b). Research exploring how best to meet this need using older adult volunteers more accustomed to technology but straddling both the digital and nondigital worlds could provide important new insights and methods for achieving these goals for healthy longevity.
As discussed previously in this chapter, the growing field of human-centered design and greater attention to participatory research and engagement of target audiences and end users should be a key facet of future research efforts. The Roadmap for AI Maturity in Health outlines key maturity indicators for assessing the design process for AI in health (Broadband Commission, 2020). Given that roadmap’s goal of putting humans at the center, there is an opportunity to augment the current list by creating an indicator that measures the representation and participation of older adults as part of the testing of datasets used to create and validate digital innovations. Using participatory design approaches to develop and understand this indicator can help improve the inclusivity and sustainability of digital designs.
CONCLUSION
Many aspects of healthy longevity are influenced by social determinants that cannot be addressed or resolved within the health system. Interventions geared toward building social cohesion and social capital within communities can con-
tribute to the cultural change needed for older adults to be more engaged in their societies. But to achieve the goals set forth in Chapter 2 and at the beginning of this chapter, these interventions also need to be paired with policies that work to combat ageism, promote social inclusion, protect the financial security of older adults, and improve opportunities for developing competence in using technology. Additionally, all of these areas would benefit from greater understanding and insight, so it will be important to ensure that translational research is funded and conducted across an array of areas to inform governments and other stakeholders when designing policies and fostering cultures of inclusion. For the findings emerging from research to be most useful and generalizable, translating and testing them in real-world settings will be a valuable addition to knowledge generation.
Older people already have meaningful roles in society as they age, but the need for new opportunities will grow with the rapid aging of populations. Meaningful engagement can yield a multiplicity of benefits for both aging populations and society. In terms of healthy longevity, challenging expectations, particularly in terms of opportunity structures, is one of the most important elements of achieving Vision 2050. Integral to the discussion in this chapter is the cross-cutting theme that the intersection of family, community and social cohesion, and equity has a vital role in achieving healthier, longer lives. Addressing these diverse but interconnected determinants holds promise for helping to achieve healthy longevity for the greatest number of people around the world. The ability of social and behavioral enablers to feed into the opportunities for healthy longevity is limitless, providing building blocks for measuring success and progress toward the world the commission envisions for 2050.
REFERENCES
African Union. 2016. Protocol to the African charter on human and peoples’ rights on the rights of older persons in Africa. https://au.int/en/treaties/protocol-african-charter-human-and-peoples-rights-rights-older-persons (accessed May 2, 2022).
Anderson, M., and A. Perrin. 2017. Technology use among seniors. Washington, DC: Pew Research Center for Internet & Technology.
Andrasfay, T., and N. Goldman. 2021. Reductions in 2020 US life expectancy due to COVID-19 and the disproportionate impact on the Black and Latino populations. Proceedings of the National Academy of Sciences 118(5):e2014746118.
Ang, S., E. Lim, and R. Malhotra. 2021. Health-related difficulty in internet use among older adults: Correlates and mediation of its association with quality of life through social support networks. Gerontologist 61(5):693–702.
Asia Health and Wellbeing Initiative. 2020. The Intergenerational Self-Help Club (ISHC) development model. https://www.ahwin.org/helpage-vietnam-ishc (accessed May 2, 2022).
Australian Government. 2015. Australia’s welfare system. https://www.dss.gov.au/sites/default/files/documents/05_2015/2015_budget_fact_sheet_-_australias_welfare_system_-_final.pdf (accessed May 2, 2022).
Avila-Parra, C., and D. Escamilla-Guerrero. 2017. What are the effects of expanding a social pension program on extreme poverty and labor supply? Evidence from Mexico’s pension program for the elderly. Washington, DC: World Bank.
Ayalon, L. 2014. Perceived age, gender, and racial/ethnic discrimination in Europe: Results from the European social survey. Educational Gerontology 40(7):499–517.
Baker, D., and H. J. Rho. 2011. The potential savings to social security from means testing. Washington, DC: Center for Economic and Policy Research.
Banerjee, D. 2021. Loneliness in older people: Spiritual practices as an alternative pathway to action, a treatise from India. Journal of Geriatric Mental Health 8(2):63–69.
Bender, A. M., I. Kawachi, T. Jørgensen, and C. Pisinger. 2015. Neighborhood deprivation is strongly associated with participation in a population-based health check. PloS One 10(6):e0129819.
Bonnet, F., J. Vanek, and M. Chen. 2019. Women and men in the informal economy: A statistical brief. Geneva, Switzerland: International Labour Office.
Borges, C. C., P. R. Dos Santos, P. M. Alves, R. C. M. Borges, G. Lucchetti, M. A. Barbosa, C. C. Porto, and M. R. Fernandes. 2021. Association between spirituality/religiousness and quality of life among healthy adults: A systematic review. Health and Quality of Life Outcomes 19(1):1–13.
Broadband Commission. 2020. Reimagining global health through artificial intelligence: The roadmap to AI maturity. Geneva, Switzerland: Broadband Commission for Sustainable Development.
Burgess, G., and K. Muir. 2020. The increase in multigenerational households in the UK: The motivations for and experiences of multigenerational living. Housing, Theory and Society 37(3):322–338.
Burnes, D., C. Sheppard, C. R. Henderson, Jr., M. Wassel, R. Cope, C. Barber, and K. Pillemer. 2019. Interventions to reduce ageism against older adults: A systematic review and meta-analysis. American Journal of Public Health 109(8):e1–e9.
Butts, D. M., L. L. Thang, A. H. Yeo, and T. Jefferson. 2012. Policies and programmes supporting intergenerational relations. New York: Secretariat of the United Nations.
Cacioppo, J. T., and L. C. Hawkley. 2003. Social isolation and health, with an emphasis on underlying mechanisms. Perspectives in Biology and Medicine 46(3):S39–S52.
Cacioppo, J. T., and S. Hawkley. 2014. Social relationships and health: The toxic effects of perceived social isolation. Social and Personality Psychology Compass 8(2):58–72.
Carstensen, L. L., and K. Chi. 2021. Emotion and prosocial giving in older adults. Nature Aging 1(10):866–867.
Carstensen, L. L., B. Turan, S. Scheibe, N. Ram, H. Ersner-Hershfield, G. R. Samanez-Larkin, K. P. Brooks, and J. R. Nesselroade. 2011. Emotional experience improves with age: Evidence based on over 10 years of experience sampling. Psychology and Aging 26(1):21.
Centre for Public Impact. 2019. Bolsa familia in Brazil. https://www.centreforpublicimpact.org/case-study/bolsa-familia-in-brazil (accessed May 2, 2022).
Chancel, L., T. Piketty, E. Saez, and G. E. A. Zucman. 2022. World inequality report 2022. Paris, France: World Inequality Lab.
Chang, E.-S., S. Kannoth, S. Levy, S.-Y. Wang, J. E. Lee, and B. R. Levy. 2020. Global reach of ageism on older persons’ health: A systematic review. PloS One 15(1):e0220857.
Changing the Narrative. 2021. Certified age-friendly employer. https://changingthenarrativeco.org/certified-age-friendly-employer (accessed May 2, 2022).
Chetty, R., M. Stepner, S. Abraham, S. Lin, B. Scuderi, N. Turner, A. Bergeron, and D. Cutler. 2016. The association between income and life expectancy in the United States, 2001–2014. JAMA 315(16):1750–1766.
Chu, C. H., R. Nyrup, K. Leslie, J. Shi, A. Bianchi, A. Lyn, M. McNicholl, S. Khan, S. Rahimi, and A. Grenier. 2021. Digital ageism: Challenges and opportunities in artificial intelligence for older adults. The Gerontologist. https://doi.org/10.1093/geront/gnab167.
Cichon, M. 2013. The social protection floors recommendation, 2012 (no. 202): Can a six-page document change the course of social history? International Social Security Review 66(3–4):21–43.
Commission on Funding of Care and Support. 2011. Fairer care funding: The report of the Commission on Funding of Care and Support. London, UK: Dilnot Commission.
Cutler, J., M. K. Wittmann, A. Abdurahman, L. D. Hargitai, D. Drew, M. Husain, and P. L. Lockwood. 2021. Ageing is associated with disrupted reinforcement learning whilst learning to help others is preserved. Nature Communications 12(1):1–13.
Cycling Without Age. 2021. Cycling without age—about us. https://cyclingwithoutage.org/about (accessed May 2, 2022).
D’Amen, B., M. Socci, and S. Santini. 2021. Intergenerational caring: A systematic literature review on young and young adult caregivers of older people. BMC Geriatrics 21(1):1–17.
Dwyer-Lindgren, L., A. Bertozzi-Villa, R. W. Stubbs, C. Morozoff, J. P. Mackenbach, F. J. van Len-the, A. H. Mokdad, and C. J. Murray. 2017. Inequalities in life expectancy among US counties, 1980 to 2014: Temporal trends and key drivers. JAMA Internal Medicine 177(7):1003–1011.
Dychtwald, K. 2021. Ageism is alive and well in advertising. https://www.aarp.org/work/working-at-50-plus/info-2021/ageism-in-advertising.html (accessed May 2, 2022).
Emmons, R. A., M. E. McCullough, and J.-A. Tsang. 2003. The grateful disposition: A conceptual and empirical topography. Journal of Personality Social Psychology 82(1):112–127.
English, T., and L. L. Carstensen. 2014. Selective narrowing of social networks across adulthood is associated with improved emotional experience in daily life. International Journal of Behavioral Development 38(2):195–202.
Every Age Counts. 2017. Drivers of ageism. https://www.everyagecounts.org.au/research (accessed May 2, 2022).
Feng, Z., J. Falkingham, X. Liu, and A. Vlachantoni. 2017. Changes in living arrangements and mortality among older people in China. SSM-Population Health 3:9–19.
Field, S., and S.-J. Fenton. 2014. More effort needs to be made to give older people a louder voice. Birmingham, UK: Birmingham Policy Commission, University of Birmingham.
Flowers, L., A. Houser, C. Noel-Miller, J. Shaw, J. Bhattacharya, L. Schoemaker, and M. Farid. 2017. Medicare spends more on socially isolated older adults. Insight on the Issues 125:1119–1143.
Fonseca, X., S. Lukosch, and F. Brazier. 2019. Social cohesion revisited: A new definition and how to characterize it. Innovation: The European Journal of Social Science Research 32(2):231–253.
Freedman, V. A., I. B. Grafova, and J. Rogowski. 2011. Neighborhoods and chronic disease onset in later life. American Journal of Public Health 101(1):79–86.
Freeman, T., H. A. Gesesew, C. Bambra, E. R. J. Giugliani, J. Popay, D. Sanders, J. Macinko, C. Musolino, and F. Baum. 2020. Why do some countries do better or worse in life expectancy relative to income? An analysis of Brazil, Ethiopia, and the United States of America. International Journal for Equity in Health 19(1):1–19.
Fried, L. P. 2016. Building a third demographic dividend: Strengthening intergenerational well-being in ways that deeply matter. Public Policy & Aging Report 26(3):78–82.
Generations United. 2021. Family matters: Multigenerational living is on the rise and here to stay. Washington, DC: Generations United.
Gertler, P., J. Heckman, R. Pinto, A. Zanolini, C. Vermeersch, S. Walker, S. M. Chang, and S. Grantham-McGregor. 2014. Labor market returns to an early childhood stimulation intervention in Jamaica. Science 344(6187):998–1001.
Giraudeau, C., and N. Bailly. 2019. Intergenerational programs: What can school-age children and older people expect from them? A systematic review. European Journal of Ageing 16(3):363–376.
Gutiérrez-Robledo, L. M., C. B. González-Rivero, L. R. Lozano-Juárez, and C. García-Peña. 2021. Approach to the opportunity cost of minor caregivers in Mexico. Cuernavaca, Morelos: Salud Publica De Mexico.
Guven, M., H. Jain, and C. Joubert. 2021. Social protection for the informal economy. Washington, DC: World Bank.
Haase, K. R., T. Cosco, L. Kervin, I. Riadi, and M. E. O’Connell. 2021. Older adults’ experiences with using technology for socialization during the COVID-19 pandemic: Cross-sectional survey study. JMIR Aging 4(2):e28010.
He, W., I. Aboderin, and D. Adjaye-Gbewonyo. 2020. Africa aging: 2020. Washington, DC: U.S. Census Bureau.
HelpAge International. 2016a. Intergenerational solidarity is helping tackle ageism in Nigeria. https://www.helpage.org/blogs/oluwayemisi-oluwole-26087/intergenerational-solidarity-is-helping-tackle-ageism-in-nigeria-1023 (accessed May 2, 2022).
HelpAge International. 2016b. Older people’s associations: A briefing on their impact, sustainability and replicability. https://ageingasia.org/older-peoples-associations-a-briefing-on-their-impact-sustainability-and-replicability (accessed May 2, 2022).
HelpAge International. 2021. Helping older people achieve financial security. https://helpageusa.org/financial-security (accessed May 2, 2022).
Hikichi, H., K. Kondo, T. Takeda, and I. Kawachi. 2017. Social interaction and cognitive decline: Results of a 7-year community intervention. Alzheimer’s & Dementia: Translational Research & Clinical Interventions 3(1):23–32.
Holman, R. 2019. Intergenerational living: French programmes pair young with old. France 24. https://www.france24.com/en/20190516-intergenerational-living-french-programmes-pair-young-old-roomates (accessed May 13, 2022).
Howse, K. 2017. Older people’s associations in East and Southeast Asia: A four country study—full report. Oxford, UK: The Oxford Institute of Population Ageing.
Jayson, S. 2018. All in together, creating places where young and old thrive. Washington, DC: Generations United.
Kamiya, Y., and S. Hertog. 2020. Measuring household and living arrangements of older persons around the world: The United Nations database on the households and living arrangements of older persons. New York: United Nations.
Kidron, E., and V. Yang. 2021. How to close the digital gap for the elderly. https://www.weforum.org/agenda/2021/01/too-old-is-simply-a-myth-tech-companies-narrow-the-digital-gap-for-the-elderly (accessed May 2, 2022).
Knodel, J., and B. Teerawichitchainan. 2017. Aging in Myanmar. The Gerontologist 57(4):599–605.
Kubzansky, L. D., J. C. Huffman, J. K. Boehm, R. Hernandez, E. S. Kim, H. K. Koga, E. H. Feig, D. M. Lloyd-Jones, M. E. Seligman, and D. R. Labarthe. 2018. Positive psychological well-being and cardiovascular disease: JACC health promotion series. Journal of the American College of Cardiology 72(12):1382–1396.
Kudrna, G. 2017. The Norwegian pension reform: An external perspective. CEPAR Working Paper 7. Sydney, Australia: University of New South Wales.
Lang, F. R., and L. L. Carstensen. 2002. Time counts: Future time perspective, goals, and social relationships. Psychology and Aging 17(1):125.
Larsen, C. A. 2014. Social cohesion: Definition, measurement and developments. Copenhagen, Denmark: Centre for Comparative Welfare Studies, Aalborg University.
Levy, B. R. 2022. The role of structural ageism in age beliefs and health of older persons. JAMA Network Open 5(2):e2147802.
Luhmann, M., and L. C. Hawkley. 2016. Age differences in loneliness from late adolescence to oldest old age. Developmental Psychology 52(6):943.
Magnan, S. 2017. Social Determinants of Health 101 for Health Care: Five Plus Five. NAM Perspectives. Discussion Paper, National Academy of Medicine, Washington, DC. https://doi.org/10.31478/201710c.
Malone, J., and A. Dadswell. 2018. The role of religion, spirituality and/or belief in positive ageing for older adults. Geriatrics 3(2):28.
Marmot, M. 2005. Social determinants of health inequalities. The Lancet 365(9464):1099–1104.
Marmot, M. 2020. Health equity in England: The Marmot Review 10 years on. BMJ 368.
Marmot, M., and R. Bell. 2018. The Sustainable Development Goals and health. Epidemiology 29(1):5–7.
Marques, B., J. McIntosh, and P. Campays. 2018. Participatory design for under-represented communities: A collaborative design-led research approach for place-making. In Handbook of research on civic engagement and social change in contemporary society. Hershey, PA: IGI Global. Pp. 1–15.
Marques, S., J. Mariano, J. Mendonça, W. De Tavernier, M. Hess, L. Naegele, F. Peixeiro, and D. Martins. 2020. Determinants of ageism against older adults: A systematic review. International Journal of Environmental Research and Public Health 17(7):2560.
Mbaka, C. 2019. Social protection is key to realising older women’s rights and sustainable development. London, UK: HelpAge International.
Mendizabal, J. 2014. The reach and impact of Bolivia’s social pension. London, UK: HelpAge International.
Mercer. 2021. Global Pension Index 2021. https://www.mercer.com/our-thinking/global-pension-index-2021.html (accessed May 2, 2022).
Mokhiber, C. 2018. Ageism in human rights law. https://www.ageinternational.org.uk/policy-research/expert-voices/ageism-in-human-rights-law (accessed May 2, 2022).
Muennig, P., B. Jiao, and E. Singer. 2018. Living with parents or grandparents increases social capital and survival: 2014 General Social Survey-National Death Index. SSM-Population Health 4:71–75.
Myers, J. 2021. These charts show the growing income inequality between the world’s richest and poorest. Geneva, Switzerland: World Economic Forum.
NASEM (National Academies of Sciences, Engineering, and Medicine). 2020. Social isolation and loneliness in older adults: Opportunities for the health care system. Washington, DC: The National Academies Press. https://doi.org/10.17226/25663.
OAS (Organization of American States). 2017. Inter-American Convention on the Protection of the Human Rights of Older Persons. International Legal Materials 55(5):985–1006.
Officer, A., J. A. Thiyagarajan, M. L. Schneiders, P. Nash, and V. De La Fuente-Nunez. 2020. Ageism, healthy life expectancy and population ageing: How are they related? International Journal of Environmental Research and Public Health 17(9):3159.
Panday, S., S. Rushton, J. Karki, J. Balen, and A. Barnes. 2021. The role of social capital in disaster resilience in remote communities after the 2015 Nepal earthquake. International Journal of Disaster Risk Reduction 55:102112.
Paris, J. 2018. Safety, health, and nutrition in early childhood education. College of the Canyons. https://open.umn.edu/opentextbooks/textbooks/908.
Putnam, R. D. 2000. Bowling alone: The collapse and revival of American community. New York: Simon and Schuster.
Singer, C. 2018. Health effects of social isolation and loneliness. Journal of Aging Life Care 28(1):4–8.
Singer, E., R. McElroy, and P. Muennig. 2017. Social capital and the paradox of poor but healthy groups in the United States. Journal of Immigrant and Minority Health 19(3):716–722.
Solar, O., and A. Irwin. 2010. A conceptual framework for action on the social determinants of health. Geneva, Switzerland: World Health Organization.
St. Ann Center. 2021. Intergenerational care for all ages & abilities in Milwaukee. https://stanncenter.org/about (accessed May 2, 2022).
Sun, R., and D. Sauter. 2021. Sustained stress reduces the age advantages in emotional experience of older adults: Commentary on Carstensen et al. (2020). Psychological Science 32(12):2035–2041.
Sunkel, G., and H. Ullmann. 2019. Older adults in the digital age in Latin America: Bridging the digital age divide. CEPAL Review 127:215–236.
Tan, E. J. 2020. How growing geographic and racial disparities inhibit the ability to live longer and healthier lives. Washington, DC: AARP.
The Economist. 2019a. A Dutch care home experiments with housing students with the old. https://www.economist.com/europe/2019/08/08/a-dutch-care-home-experiments-with-housing-students-with-the-old (accessed May 13, 2022).
The Economist. 2019b. The shift index. https://ageingshift.economist.com (accessed May 2, 2022).
The Lancet and Financial Times Commission. 2021. Digital technologies: A new determinant of health. Journal of Medical Internet Research 23:e18286.
Tomer, A., L. Fishbane, A. Siefer, and B. Callahan. 2020. How broadband can deliver health and equity to all communities. Washington, DC: Brookings Institution.
UK (United Kingdom) Office for National Statistics. 2019. Measures of national well-being dashboard. https://www.ons.gov.uk/peoplepopulationandcommunity/wellbeing/articles/measuresofnationalwellbeingdashboard/2018-04-25 (accessed May 2, 2022).
Umberson, D., R. Crosnoe, and C. Reczek. 2010. Social relationships and health behavior across the life course. Annual Review of Sociology 36:139–157.
UN (United Nations). 2010. Strengthening older people’s rights: Towards a UN convention. Geneva, Switzerland: United Nations.
UN. 2013. Convention on the rights of persons with disabilities. Geneva, Switzerland: United Nations.
UN. 2018. Old age: Responding to a rapidly ageing population, The report on the world social situation. Geneva, Switzerland: United Nations.
UN. 2019a. Living arrangements of older persons around the world. New York: United Nations Department of Economic and Social Affairs.
UN. 2019b. Why are digital skills critical for older persons? Geneva, Switzerland: United Nations.
UN. 2020a. Care in Latin America and the Caribbean during the COVID-19: Towards comprehensive systems to strengthen response and recovery. Geneva, Switzerland: United Nations.
UN. 2020b. World social report 2020: Inequality in a rapidly changing world. Geneva, Switzerland: United Nations.
UN. 2021. Sustainable Development Goals indicators. https://unstats.un.org/sdgs/metadata (accessed May 2, 2022).
UN General Assembly. 1948. Universal declaration of human rights. UN General Assembly 302(2):14.
UN Women. 2021. The United Nations in Lebanon launches fund to support women’s rights organizations to enhance women’s participation in the Beirut port explosion response and recovery process. https://arabstates.unwomen.org/en/news/stories/2021/06/the-united-nations-in-lebanon-launches-fund-to-support-womens-rights-organizations#_ftn1 (accessed May 2, 2022).
UN Women, CARE, UN ESCWA (United Nations Economic and Social Commission for Western Asia), ABAAD (Resource Centre for Gender Equality), and UNFPA (United Nations Population Fund). 2020. Rapid gender analysis of the August 2020 Beirut port explosion: An intersectional examination. Geneva, Switzerland: United Nations.
UNECE (United Nations Economic Commission for Europe)/European Commission. 2018. Active Ageing Index (AAI) in non-EU countries and at subnational level. Geneva, Switzerland: United Nations.
United for All Ages. 2018. Mixing matters: How shared sites can bring older and younger people together and unite Brexit Britain. Happisburgh, UK: United for All Ages.
WHO (World Health Organization). 2009. Social determinants of health and well-being among young people. Geneva, Switzerland: World Health Organization.
WHO. 2020. Decade of healthy ageing: Baseline report. Geneva, Switzerland: World Health Organization.
WHO. 2021a. Global report on ageism: Executive summary. Geneva, Switzerland: World Health Organization.
WHO. 2021b. Social isolation and loneliness among older people: Advocacy brief. Geneva, Switzerland: World Health Organization.
WHO. 2022a. Ageism in artificial intelligence for health: WHO policy brief. Geneva, Switzerland: World Health Organization.
WHO. 2022b. Social determinants of health. https://www.who.int/health-topics/social-determinants-of-health#tab=tab_1 (accessed May 2, 2022).
WHO Africa. 2021. WHO AFRO and HelpAge International partnering to combat ageism in the African region. https://www.afro.who.int/news/who-afro-and-helpage-international-partnering-combat-ageism-african-region (accessed May 2, 2022).
WIEGO (Women in Informal Employment: Globalizing and Organizing). 2022. Social protection for informal workers: Trends and changes extending social protection for informal workers in Togo. Manchester, UK: Women in Informal Employment: Globalizing and Organizing.
World Bank. 2021. World Bank, Japan support promoting community based care for the elderly in Vietnam. https://www.worldbank.org/en/news/press-release/2021/09/29/world-bank-japan-support-promoting-community-based-care-for-the-elderly-in-vietnam (accessed May 13, 2022).
Yim, J.-H., H.-J. Lee, and J.-H. Lee. 2020. A study on digital divide influence factors of the elderly: Comparison between baby boomer and elderly. The Journal of the Korea Contents Association 20(9):475–485.










































