Proceedings of a Workshop
INTRODUCTION1
The COVID-19 pandemic continues to have a profound impact on health care systems, economies, and societies around the world. In the United States, the pandemic shone a harsh light on existing weaknesses in the health care system, ranging from significant racial and ethnic disparities in care to flaws in our public health system, while creating a new set of challenges related to caring for people of all ages and all stages of serious illness. The pandemic also offers opportunities to apply important lessons learned to improve care. In an effort to explore the impact of the pandemic on caring for people with serious illness, the National Academy of Sciences, Engineering, and Medicine’s Roundtable on Quality Care for People with Serious Illness hosted a three-part virtual public workshop, Caring for People with Serious Illness During the COVID-19 Pandemic: A Workshop on Lessons Learned and Future Directions. The three webinars were held on November 8, 18, and 30, 2021.
___________________
1 The planning committee’s role was limited to planning the workshop, and the Proceedings of a Workshop has been prepared by the workshop rapporteurs as a factual summary of what occurred at the workshop. Statements, recommendations, and opinions expressed are those of individual presenters and participants, are not necessarily endorsed or verified by the National Academies of Sciences, Engineering, and Medicine, and should not be construed as reflecting any group consensus.
The first webinar explored the initial response to the pandemic on the part of public health and the health care teams providing care to people with serious illness in hospitals and the community. The second webinar focused on the impact of the pandemic on the health care workforce and the use of telehealth. The third webinar examined the issue of communicating with the public about health emergencies, with a particular eye to specific populations, such as pediatrics and minority populations. The final session explored the lessons learned from the perspective of policy opportunities to improve care for people with serious illness.
This Proceedings of a Workshop summarizes the workshop’s presentations and discussions. The speakers, panelists, and workshop participants presented a broad range of views and ideas. Box 1 provides a summary of lessons learned and suggestions made by individual workshop participants based on the experience of providing care to people with serious illness during the COVID-19 pandemic. Appendixes A and B contain the workshop Statement of Task and the workshop agenda, respectively. The speakers’ presentations (as PDF and audio files) have been archived online.2
___________________
2 For additional information, see https://www.nationalacademies.org/event/11-08-2021/impact-of-and-response-to-the-pandemic-webinar-1; https://www.nationalacademies.org/event/11-18-2021/recovery-and-resilience-webinar-2; and https://www.nationalacademies.org/event/11-30-2021/prevention-and-preparedness-webinar-3.
WEBINAR ONE
James Tulsky, of Dana-Farber Cancer Institute, Brigham and Women’s Hospital, Harvard Medical School, and co-Chair of the Roundtable, opened the first webinar by noting that the world turned upside down in the spring of 2020, and for those who work in palliative care or other serious illness care, it was a time of great need, reflection, and value. “All of the things that we had been working on for so long suddenly were in the minds of everyone—the role of family and social isolation, the need for high-quality decision making in the face of serious illness, the attention to symptoms and comfort in the face of illness that may be incurable, and the importance of high-quality communication in every facet of what we do,” observed Tulsky. “Suddenly, those of us who focused on serious illness care felt thrust into the middle of everyone’s plans, and our value was apparent in plain sight,” he added.
In response to an inadequate supply of personal protective equipment (PPE) for staff, Tulsky recalled ordering baby monitors online so that he and his colleagues could monitor patients in the COVID-19 palliative care unit remotely. He also remembered the frantic family meetings and the pain of trying to describe the situation to family members who could
only imagine what their loved ones were going through. “I will also never forget celebrating Marge, the 96-year-old woman who was admitted to our COVID palliative care unit and survived her bout with the virus,” Tulsky shared. “Marge left the hospital to a cheering crowd,” he added.
Tulsky pointed out that the pandemic has upended all aspects of how he and his colleagues do their work. It has exacerbated the challenge of dealing with patients with new chronic conditions and those who had existing conditions and missed the care they would have normally received. The pandemic, he added, amplified the tremendous disparities that exist in the care that health systems provide. As a final note, Tulsky remarked that he is grateful that the broader health care workforce now values and appreciates the work of the palliative care team, but he wished it had not taken a pandemic to make that happen.
In her overview of the workshop series, Planning Committee Co-Chair Susan Elizabeth Wang, National Lead, Palliative Care for Kaiser Permanente, said that in addition to the more than 750,000 Americans who died from the SAR-CoV-2 virus,3 up to one-quarter of those affected have sought care for “long COVID” symptoms4 that include memory loss, breathlessness, and fatigue. She added, “We recognize that people without COVID also require care for advanced illness, and the pandemic’s strain on our health systems has affected access to treatment for these individuals.”
It has become clear that a single, unified experience for this national tragedy does not exist, observed Wang. Health disparities are prevalent, with Indigenous American, Black/African American, Hispanic, and Pacific Islander individuals having a death rate of double or more than that of white and Asian American individuals.5 Older adults and people with chronic illness suffer increased complications, and regional variation has been substantial. People living in rural areas have had a much higher mortality rate than people in urban areas. Because of these disparities, health equity became a necessary priority in planning the workshop, as did focusing on novel programming, workforce, telehealth, and policy levers that will help the nation prepare for a better future.
___________________
3 Numbers reflect total deaths at the time of the first webinar. By the end of 2021, total deaths surpassed 800,000. https://ourworldindata.org/coronavirus/country/united-states (accessed March 10, 2022).
4 Additional information about long COVID and its symptoms is available at https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects/index.html (accessed March 10, 2022).
5 See https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/racial-ethnic-disparities/index.html (accessed March 10, 2022).
Wang said that one of the many important lessons she has learned in living through the pandemic as a physician is that people create recovery. “Communities recover when people choose to commit, to reconnect, and rebuild,” Wang observed. Explaining that the first webinar in the series would focus on some of the many innovative responses to the immediate impact of COVID-19, Wang characterized the workshop as “our call to reflection and shared learning to improve the lives of people with serious illness and those who care for them.”
The Immediate Impact of the Pandemic
The first webinar began with a keynote address by Harvey Fineberg, president of the Gordon and Betty Moore Foundation. Fineberg drew on his experience as chair of the National Academies Standing Committee on Emerging Infectious Diseases and Twenty-First Century Health Threats.
Keynote Address
Fineberg began by pointing out that pandemics have occurred historically at irregular intervals, from decades to a century or more. Because they are so infrequent relative to a human lifetime, we have relatively few instances to study them but a long time to think about them after the fact. That infrequent nature tends to encourage overconfidence in terms of understanding, anticipation, and the ability to respond. In addition, Fineberg pointed out that the long interval between recent pandemics promoted neglect of the public health infrastructure that is so crucial to pandemic response.
While emerging zoonotic infections (diseases that are transmitted between species) often cause pandemics, whether they do so depends on the specific infectious agent and the particular setting in which they emerge. For example, the first SARS outbreak early in the twenty-first century affected various places and caused severe illness, but if it had emerged in extremely densely populated areas, such as New Delhi and Kinshasa, instead of Toronto and Singapore, the impact would have been very different. Noting the high degree of uncertainty surrounding any pandemic, Fineberg asked a series of questions: “Who among us could state with absolute confidence what the course of the pandemic we are now experiencing will be throughout the winter that we are about to face? Will the immunizations and other measures lead to a suppression of disease, and how effective will our new
treatments be to suppress the development of serious illness? Has it played out already as much as it is going to, or is this virus not quite done with all the tricks, metaphorically, it has up its sleeve in terms of variants and other developments?”6 All of this uncertainty, layered on top of the infrequency of a pandemic, makes coping with it an ongoing challenge, explained Fineberg.
Fineberg described six required elements for a successful response to a public health emergency. The first is leadership. Any crisis, includes both the demeanor and content of leadership. The public looks to leaders for confident, calm, and clear communication and accurate assessments that help everyone understand where things stand and how the nation is responding. In Fineberg’s view, leadership should take advantage of the best available evidence, make sound decisions, account for fairness, and, most of all, always keep the welfare of the entire population in mind.
The second element is the significant role of science, which provides the evidence that represents the soundest basis for decision making in the face of a pandemic. Fineberg noted that early in the pandemic, U.S. leadership played down its seriousness, dismissed the likely consequences, provided false reassurance, and touted treatments that proved to be ineffectual.
Leadership and science are two important foundations for the third element, which is public trust, understanding and action. Public trust has eroded over time, he explained, which has contributed to the lower proportion of the U.S. adult population receiving the vaccine, as compared to other nations such as Canada and Australia.
Fineberg identified the fourth key element as a sound pandemic response strategy. Good leadership that relies on science and has the public’s trust has to translate those assets into a strategic response that encompasses ways to care for those who are ill, interrupts the speed at which an illness spreads, and puts in place the conditions that will minimize the consequences over time. Strategically, it is difficult to accomplish a national response in a country like the United States, where sovereignty has never fully been resolved between the national government and the individual states, explained Fineberg. This caused questions as to where the authority rested when the nation needed to respond with urgency and consistency, and states were forced to compete with one another for the limited initial supplies of PPE and ventilators. Managing this foundational challenge
___________________
6 Within a month of Fineberg’s remarks, the Omicron variant emerged and swept across the globe.
became even more difficult given the global impact of the pandemic and the competing interests and strategies among the world’s nation-states.
The fifth element is adequate resources to enact the strategy, and this was a serious shortcoming in the initial U.S. response to the pandemic. “I need not remind any of you who were caring for patients in the first months of the pandemic how stressful it was in the absence of adequate protective equipment and basic supplies,” said Fineberg. In contrast, the nation spent billions of dollars on developing vaccines and additional billions developing effective, convenient, and rapid home-based testing.
The final element is the ability to implement the strategic response on the ground, which takes a different type of leadership. The United States, Fineberg said, benefited tremendously from its long history of individual volunteerism and readiness to pitch in during an emergency. The health care system, designed for routine conditions and pulse emergencies, was overwhelmed and overstressed by the pandemic’s long-term, emergent, and severe conditions.
Fineberg identified five consequences of not having those six elements in place during the COVID-19 pandemic:
- the substantial number of patients experiencing the acute and long-term consequences of infection;
- the disruption in care affecting patients who had existing serious illnesses and the adaptation required to manage the care of all patients during the pandemic;
- the stress on health care providers, health care institutions, and the health care system and the strain for continuous obligation and uncertainty;
- the disparities in care that the pandemic has exacerbated and revealed as a severe deficiency in the nation’s health care system; and
- the disruption of the larger social context, economic system, and capacity to provide necessary social services and support systems for families and the ability of communities to function, all of which complicate the ability of the health care system and health professionals to provide the care that patients need.
Together, these make the workshop discussions so important for taking stock of lessons from the pandemic, concluded Fineberg. “How can we take those lessons and apply them in a consistent and effective way to improve the care of patients with serious illness?” he asked.
The Lived Experience
Jarrod A. Carrol, a geriatrician with Kaiser Permanente, offered his perspective on what it was like to care for people with serious illness during the pandemic. Carrol explained that COVID-19 presented an unrelenting challenge that forced changes in how he went about his daily routine, saw his patients, and interacted with their families. Carrol offered the word “change” as an acronym for what he learned during the pandemic.
“C,” he said, stands for communication, which the pandemic affected significantly. Beginning in early 2020, COVID-19 quickly paralyzed the normal routes of communication, affecting the daily routine and environment that is integral to successfully managing individuals with dementia in the clinic in which he works. Changing communication techniques, he noted, was no easy task for this patient population or their families. He and his colleagues launched a proactive outreach initiative, led by the clinic’s social worker and case manager, to reach out to patients and their families to help them navigate the challenges they were facing.
Carrol explained that as Kaiser Permanente focused its energies on virus containment efforts, his work shifted from the clinic to the nursing home setting, where he witnessed even more of the detrimental effects the pandemic was having on communication. The resulting lockdowns that closed nursing facilities to visitors affected his patients physically, mentally, and emotionally. Carrol recounted when a patient told him he felt like a prisoner or a hostage. “I was overwhelmed, but I spent some additional time with him explaining why we were taking the measures that we were taking,” said Carrol. “I do not think he quite understood it that first day, but over time, I think he grew to understand we were committed to his health.”
Slowly, the nursing facility was able to transition to a virtual platform for providing care, but in the interim, families were waiting anxiously to receive updated information about their loved ones. Families also had to participate in care planning and life-and-death decisions via telephone, even in instances where COVID-19 was not the primary concern. One shortcoming of the virtual platform, Carrol pointed out, was losing nonverbal communication and the ability for family members to stand by their loved ones and hold their hands during these discussions. As a result, he had to function as the critical communication link to the families.
Carrol explained that the “H” represents hope and health—the hope that as the spread and impact of the virus continued, there would be eventual containment, a vaccine, and a return to health. Over time, the conversation
shifted from when the pandemic would end to hope that vaccine would lead to health and healing. Thinking about hope and health, he said, reminds him of an encounter in which he had to convince a patient who needed kidney dialysis and her family that she needed to go to the hospital to receive necessary treatment for her condition if she hoped to regain her health.
The “A” in “change,” said Carrol, stands for advocacy for the aging and seriously ill, which became even more important during the pandemic given its disproportionate effect on older adults and those with chronic illness. This vulnerable population faced a double risk from the virus and the effects of isolation on their physical and mental health. “Tying back to communication, many patients in nursing homes lost their bedside advocate, so we had to be their advocate even more than usual,” said Carrol. Advocacy also included proactive outreach programs that many clinics, including his, employed to help monitor chronic disease and even conduct home visits. In addition, he and his colleagues realized that many of those with serious illness are somewhat tucked away in their homes or nursing facilities, away from the main view of health care. “We had to advocate for their care by making sure that they were considered when we were eventually rolling out the vaccine,” said Carrol. He developed a list of homebound patients to make sure they received the vaccine when their time came. “It was important for us to stand as advocates for the patient and continue to grow the patient, doctor, and family relationship,” he added.
Carrol explained that the “N” in “change” was particularly important to him on a personal level, because it calls out the importance of nurturing the health care team. He recounted how, as the pandemic continued, and he and his colleagues focused on caring for their patients, they often neglected caring for themselves. “If we did not take care of ourselves, we could not take care of anyone else, including the seriously ill who trust us,” said Carrol.
The “G,” he continued, stands for the greater good. What most people thought initially to be short-term changes eventually became a prolonged and huge task that weighed heavily on everyone, even with the knowledge that protective measures were saving lives. “We had to focus on the fact that there is no ‘I’ in ‘team,’ ‘we,’ or ‘success.’ We had to cooperate and focus on the greater good by modeling what we wanted our patients and their families to follow,” said Carrol.
The “E” stands for equity and empowerment. As Fineberg emphasized in his presentation, the pandemic further exposed existing inequities and highlighted that health equity is still not a reality. Addressing those ineq-
uities requires empowerment, one aspect of which included using virtual platforms to connect with patients, families, and caregiver groups throughout the country in an effort to address concerns such as vaccine hesitancy. Carrol concluded that change is the only constant in life.
Discussion Session
Session moderator Judy Salerno, president of the New York Academy of Medicine, opened the discussion session, which included the two previous speakers and Brynn Bowman, chief executive officer of the Center to Advance Palliative Care. Salerno reflected on the many disruptions the pandemic triggered, while considering the ongoing need to be disruptive in health care. She asked Fineberg and Carrol to identify some of the durable changes in health care that may result from these disruptions. Fineberg commented that health care needs disruptions that are thoughtful, important, and intentional, yet the pandemic-triggered disruptions were none of those. Perhaps one disruption to consider is the widespread adoption of telemedicine and telehealth and their ability to allow patients to interact meaningfully at a distance with their clinicians. While not a substitute for face-to-face interaction, telehealth proved to be an important complement to care that can engage patients in a reinforcing and comforting manner.
Brynn Bowman observed that there was a rapid evolution and a great deal of creativity around how to best use telehealth to extend the scarce resources that many palliative care teams deal with regularly. For example, palliative care specialists were able to use virtual platforms to talk to patients in the emergency department (ED) and nursing homes, extending their reach beyond their local institution or clinic. Bowman pointed out that she expects that palliative care will adapt and integrate telehealth for long-term use. She also hoped that the pandemic will disrupt how health care systems think about staff members’ emotional well-being, since business-as-usual solutions and resourcing are not going to be sufficient. Bowman shared her optimism that the new clinical partnerships developed during the pandemic would endure, particularly those that led to what appears to be a lasting increase in consults requested of specialty palliative care teams. The implication, she added, is that “we have to think about what it means to resource palliative care teams to be able to provide services to a large number of patients.”
Carrol agreed that the widespread use of virtual platforms will continue, particularly since this allows clinicians to see patients where they are
and view their everyday experiences. “When we utilize this opportunity to see patients where they are, we actually learn so much more about them and understand obstacles that may be present in the home setting,” said Carrol. He also agreed with Bowman about the huge growth in attention paid to the mental and physical well-being of caregivers and providers.
Regarding lessons learned from COVID-19 that might influence health professional education, Fineberg said that the pandemic has reinforced the value of interprofessional education and the role it can play to make care more effective. Carrol commented that at his institution, the pandemic experience has renewed interest in wellness and taking care of the medical students and fellows. In addition, it has highlighted the importance of incorporating a focus on health inequities and their relationship to the social determinants of health in medical education. “If we do not train trainees to be able to appreciate those differences, then they will not be truly empathetic providers to take care of those patients,” said Carrol. “We have to be able to listen to the patient and know where they are in order to truly be able to provide care.”
Fineberg commented that the pandemic has also emphasized the importance of pre-positioning protocols and networks to enable real-time clinical and public health research that produces evidence in a scientifically reliable way about what does and does not work in an emergency. Fineberg noted that this calls out the difference between plans and preparedness. Preparedness, he said, requires a significant degree of readiness, on-the-ground resources, adequate equipment, real tests through simulated experience to identify the weaknesses in the system, and pre-positioning networks for both public health and community-based investigation.
Posing a question from a participant, Salerno asked Bowman for the operational definition of serious illness. Bowman replied that it is a life-limiting illness that negatively affects quality of life and function or excessively burdens caregivers (Kelley and Bollens-Lund, 2017). Bowman addressed another participant question about fee-for-service payment and the delivery of care for complex and persistent episodes of illness, including long COVID. “Fee-for-service is poorly matched to the needs of patients who have medical illness and complex needs over time,” observed Bowman.
Bowman explained that fee-for-service health care makes it difficult to collaborate with social workers or community service agencies to address the social determinants of health that Carrol discussed. “When you look at examples of organizations and entities that are leaning more into value-based care or have capitated arrangements for the care of patients with serious illness … we start to see some of these flexibilities that allow for adap-
tive clinical relationships with very sick patients over time,” said Bowman. Carrol agreed with Bowman and noted a likely increase in the number of patients with serious illness because a large majority of individuals delayed important medical screenings during the pandemic. Fee-for-service care, he noted, does not appear to be appropriately resourced to address the resulting need for repeat visits associated with serious illness.
Fineberg pointed out that the deficiencies of a fee-for-service system did not originate during the COVID-19 pandemic, but they were more visibly exposed by the heightened demand for care of patients who are seriously ill and need long-term, comprehensive care. He also noted that fee-for-service payment models work contrary to the ideal of putting the patient first in providing compassionate, continuous, and comprehensive care. From a practical point of view, one potential approach to rectifying what has proven to be a difficult system to change may be to separate how patients pay from how health systems compensate or incentivize some subsets of clinicians.
A workshop participant asked if there is some aspect of the capitation system employed in the Program of All-Inclusive Care for the Elderly (PACE) model that produces better outcomes in a seriously ill, older population. Carrol said that one important aspect is that PACE tends to treat fewer patients, which seems to result in a stronger connection with health care team members. He noted that PACE programs were able to quickly transition to keep their patients at home, which may have been due to providers being able to quickly get patients’ buy-in based on their close relationships. “It highlights the importance of having a medical home and of having a medical director that is truly connected to the patients and their families, because if we get that buy-in, they will model our behavior,” said Carrol.
Salerno then asked Bowman to talk about how palliative care teams functioned when they had to talk to patients and families about goals of care in such a profoundly disjointed manner. Bowman said that her organization conducted surveys of palliative care programs and asked the teams how they were adapting their service delivery in response to the pandemic and the impact on patients and families, colleagues, and organizations; almost every palliative care program had rapidly scaled its use of telehealth.7
Bowman pointed out that three-quarters of the programs also reported that they started new interventions or services to address the emotional well-being of their non-palliative-care colleagues. “That was work that palliative care teams were owning and innovating around,” she said. About the same
___________________
7 See https://www.capc.org/events/recorded-webinars/briefing-palliative-care-outlook-in-2021-results-of-a-national-survey (accessed March 10, 2022).
proportion of programs reported that they were also leading the efforts within their organizations to ensure that COVID-19 patients were able to talk about their goals of care, and some palliative care teams quickly began teaching other clinical colleagues to have these conversations. The fact that this was occurring, she added, points to the need to include talking about goals of care or managing symptoms in the core skill sets taught to clinicians who will be working with patients with serious illness.
Bowman noted that the surveys also revealed that palliative care teams expanded their presence in the ED and intensive care units (ICUs). More than half of the programs reported that they had worked with their organizational leadership to design the crisis response strategy in the early days of the pandemic. “That makes sense because palliative care teams are expert at acting in an environment of uncertainty to relieve suffering and help patients cope and help support patients and families through complicated decision making,” remarked Bowman.
Salerno wondered if the principles of palliative care could help address the needs of patients dealing with long COVID. Bowman replied that this is an area that needs more research to understand what these patients are grappling with, how long those symptoms will last, and what the best ways to support families will be. Carrol, who is now back in the memory clinic, said he is seeing many changes in his patients because of the neurological effects of COVID-19 and its impact on memory. Carrol then pointed to the importance of checking in with patients and families who have lost loved ones to COVID-19. He suggested that neglecting to address their mental and emotional decline would lead to more long-term effects on COVID-19 patients and those who experienced loss during the pandemic.
Returning to the issue of social determinants of health and health equity, a workshop participant asked if there is an opportunity to train a substantial number of leaders in each clinical area on topics such as urban planning, community organizing, housing, and economic policy as a means of addressing the social determinants of health. Fineberg called out the need for individuals trained in medicine who will devote their intellectual and professional lives to doing exactly that, namely to serve as bridge builders between the social and policy worlds and the clinical and patient care worlds. He added that he believes that leadership emerges not from a role but from action. “It is not the formal authority that anyone brings to a situation that signifies their leadership,” he said. “It is what they do in any role to bring others to do things that are necessary and require working together and inspire people to do more than they would otherwise do.”
Asked for concluding thoughts, Carrol said while it appears the nation is turning the corner, we still have much to learn and understand about how the health system can adapt to address the changes wrought by the pandemic so that when the next one arises, the next generation of providers will be better prepared. Bowman said her takeaway is that palliative care teams have been able to adapt quickly to prevent as much suffering as possible, despite being small or nonexistent in many health care organizations. As a result, patients served by those organizations did not have the benefit of those services, nor were the treating clinicians able to lean on their palliative care colleagues. “We have to think about what that variability in access and preparedness means coming out of COVID-19,” she said. Fineberg concluded the discussion by observing that learning and keeping an open mindset while doing can be empowering in circumstances that can sometimes seem overwhelming.
Innovative Early Responses to the Pandemic
The workshop’s second panel session began with a brief video montage showcasing five examples of innovative approaches that facilitated high-quality care for people with serious illness and their families during the early days of the pandemic.
- Terri Maxwell, from Turn-Key Health, spoke about the organization’s use of Zoom meetings to bring together patients, family members, and clinicians to discuss goals of care using the serious illness conversation guide to develop an advance care plan.
- Tara Floyd and Simmy King, from Children’s National Hospital, discussed how the hospital expanded its care population to include young adults with COVID-19 to relieve pressure on other hospitals in the Washington, DC, area. This required the institution, which specializes in pediatric care, to develop a curriculum to train all of its nurses on how to care for young adults. It included a review of age-specific competencies and advanced cardiac life support and training modules on oxygenation and safe medication practices.
- Meaghann Weaver, from Children’s Hospital and Medical Center and the University of Nebraska Medical Center in Omaha, noted that it serves a primarily rural population and had already implemented telehealth capabilities prior to the pandemic to offer longitudinal care for patients in hospice. It supported home hospice
- Hannah Coyne and Patrick Coyne, from the Medical University of South Carolina, discussed Code Lavender, a program they used to provide peer support for team members.8 It included a virtual debriefing where staff members could speak with chaplains, therapists, and the bereavement coordinator about their experiences. On the patient care side, the institution provided iPhones so that patients could FaceTime with family members when visitors were no longer allowed into the facility.
- Breanna Burke, a community health worker (CHW) in Bristol, TN; Nubia Armenta, a community health specialist in Huntington Beach, CA; and Claude Clements, a CHW in Philadelphia, PA, discussed how the COVID-19 pandemic affected their communities and how they were able to continue working with their patients to meet their needs. Clements noted that he had four relatives on ventilators and three who died from COVID-19. Armenta pointed out that one of the most significant impacts on her community and family was unemployment. Burke explained that her organization provided masks and gloves to the local food pantry so that it could reopen and help patients and the community. Armenta noted that the pandemic triggered a widespread increase in depression and anxiety, which added to their existing patient load. In her view, the most effective resource CHWs provided was someone to talk with about the issues and fears community members were facing.
teams caring for not only children but also adults. During the pandemic, health care teams were able to leverage existing telehealth capabilities to ensure continuity in care for children with complex needs. The institution also collaborated with colleagues in New York City to provide additional telehealth training for adult and pediatric palliative care at the height of the pandemic.
The Role of Hospice during the Pandemic
The session opened with remarks by Carla Davis, chief executive officer of Heart of Hospice during the pandemic and currently senior vice president of hospice operations at LHC Group, which recently acquired
___________________
8 See https://consultqd.clevelandclinic.org/code-lavender-offering-emotional-support-holistic-rapid-response (accessed March 10, 2022).
Heart of Hospice.9 Davis explained that Heart of Hospice’s mission was to serve every dying patient regardless of the complexity and cost of that care. “We try to knock down barriers to people getting the care they need and deserve,” she explained. When COVID-19 arrived, it made sense that her organization would serve as many COVID-19 patients as needed to help its communities and its health care systems.
During the pandemic’s first year, Heart of Hospice served over 780 COVID-19 patients, including 7 percent of all those who died of COVID-19 in Louisiana.10 Davis pointed out that New Orleans was particularly hard hit and patients were in hallways, parking lots, the convention center, and even in three of the city’s parks. During that time, the organization’s medical director proposed creating an inpatient hospice unit (for COVID-19 patients), something that normally takes 2–3 years to set up. While acknowledging that this was a “completely insane idea,” Davis said she and her colleagues set out to make it a reality, receiving strong support from the state that included granting regulatory approval a day after receiving the proposal. Eight days later, the first patient arrived. At first, Louisiana only granted a 90-day approval, so Heart of Hospice relied solely on volunteers for the first 90 days. Although people were scared in the early days of the pandemic, staff from its locations nationwide volunteered and came to New Orleans.
One lesson she learned from this experience aligned with Fineberg’s earlier comment that leadership emerges from action. Leadership during a crisis, she noted, requires the same skills as leadership outside of a crisis, except that it is more intense and needs to be more intentional and more focused. For her, the most important part of leadership was making sure that her team was going to be safe.
Another lesson Davis learned about leadership was the importance of transparency and leading with vulnerability. “There were times when I was scared,” she said, noting that she contracted COVID-19 from her 84-year-old mother. Part of being transparent is to communicate effectively, she added, so she ensured there was an established approach for communicating often with staff, including weekly virtual town halls and weekly e-mails. She also learned that improbable does not mean impossible when the team comes together to support a vision and that, in chaos, it is important to keep or establish a routine and structure that can provide comfort in the storm.
___________________
9 See https://www.heartofhospice.net (accessed March 10, 2022).
10 See https://www.heartofhospice.net/covid-19-response (accessed March 10, 2022).
The PATCH-24 Service at Mount Sinai
Claire Ankuda, assistant professor of geriatrics and palliative medicine at the Icahn School of Medicine at Mount Sinai, described the model of rapid telephonic and in-person ED palliative care outreach that she and her colleague, Christopher Woodrell, developed to meet the needs of their health system during the spring 2020 COVID-19 surge (Ankuda et al., 2020). The two palliative care specialists built this service, known as “PATCH-24,” to prevent calls to their overwhelmed clinicians from going to voicemail and ensure that no one would have to wait more than 30 seconds to reach a trained palliative care clinician.
During the day, medical students operated PATCH-24. They would send a group text to a primary geriatric fellow and attending physician to see if they could take a call. If neither was available, the medical student would reach out to a backup pool comprising physicians, nurse practitioners, and on occasion, volunteers nationwide. If none of them were available, the students would contact Ankuda or Woodrell. Between two to four outpatient geriatrics and palliative care fellows helped cover the PATCH-24 hotline at any given time (Chopra et al., 2021).
Ankuda described how the volume of cases rose dramatically between March and April of 2020, and PATCH-24 was able to accommodate that increase11 (see Figure 1). Overall, PATCH-24 handled nearly 1,000 patients over that time period (Ankuda et al., 2020).
Ankuda shared lessons learned from the PATCH-24 experience. First, telephonic consultation, if properly integrated, can effectively extend in-person services. Ankuda pointed out that it was important to have people who could help to identify patients for whom the service was appropriate. In addition, while she and her colleagues could certainly speak to families in a one-time context, these conversations often needed to be longitudinal. “We needed to be able to hand the communication back to our primary consult service if needed,” explained Ankuda.
Ankuda pointed out that the experience underscores the importance of having an in-person presence and local champions. Ankuda noted that some other institutions that started similar call lines did not get calls, and she hypothesized that the reason PATCH-24 worked in her health system was that it always had an on-the-ground approach. For example, one day
___________________
11 The PATCH-24 line was available to 6 hospitals within the Mount Sinai Health System throughout New York City.
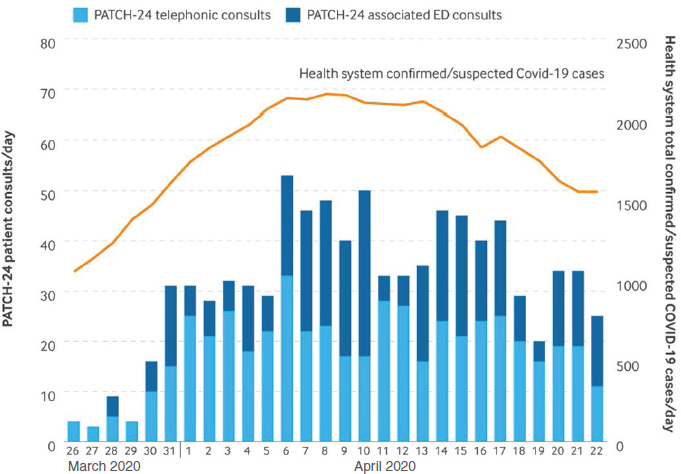
NOTES: PATCH-24 telephonic consults were directly received by frontline physicians. PATCH-24–associated ED consults were referred to an in-person PATCH-24 physician in the ED, who then called the patient’s family.
SOURCE: As presented by Claire Ankuda, November 8, 2022; Ankuda et al., 2020.
early in the pandemic, the call line went quiet even though the hospitals were overwhelmed. “Our clinical chief, in talking to the emergency room, soon realized they just did not have time to pick up the phone,” she explained, “so we started sending one of our physicians and a fellow into the emergency rooms from 11 a.m. to 7 p.m.”
For those hospitals in the health system who were less familiar with palliative care, Ankuda’s team sent palliative care physicians to build a bridge to PATCH-24. They helped coach other clinicians to understand when it was appropriate to use the call line, while also building familiarity with palliative care.
Ankuda acknowledged that this staffing model was not sustainable, even for a health system such as hers that has a substantial palliative care service. PATCH-24 relied predominantly on physicians, including people like herself, who normally focus on research and those who usually work in outpatient or inpatient services that closed during the pandemic and could
be redeployed. PATCH-24 also relied on a large volunteer base, which was possible because New York State enacted emergency laws and the hospital had protocols that allowed her team to rapidly onboard people nationwide, which was not possible in other states.
Noting that other models are feasible, Ankuda pointed out that although PATCH-24 intentionally overstaffed its program to prevent calls going to voicemail during the extreme surge in COVID-19 patients, a much simpler model with one or two physicians or nurse practitioners would be able to handle a substantial call volume. Ankuda explained that her team learned to be creative about using available health care and social service professionals. For example, two of the health system’s hospitals had a large number of residents who were looking for a role. “We were able to work with our social workers to create a training module where they all learned about New York State’s surrogate decision-making laws, which are a bit complex, and also learned how to have conversations with patients about health care proxies,” said Ankuda. Once trained, the program deployed these residents to EDs, where they saw every patient. If the patient had the capacity to make decisions, the residents asked them who they wanted to be their health care proxy, helped them complete the appropriate paperwork, and placed it in their chart. If the patient was not capable, the resident would search for someone who could serve in that role, identify the appropriate person, and document their contact information.
One surprising lesson, observed Ankuda, was that telemedicine provided an excellent platform for teaching. Her health system’s communication team developed communication scripts for talking about COVID decision making in low-acute, medium-acute, and high-acute situations. The scripts would then be available for the fellows while they were on the phone with family members, while the attending would listen and provide coaching in real time via text or chat on the computer. This approach proved to be a good model for receiving feedback, said Ankuda, and the fellows reported that the autonomy this approach allowed them to step outside their comfort zone and was beneficial for their learning. “They really appreciated that opportunity, and we could not have done this without our fellows,” she said.
Ankuda explained that overcommunication played a vital role in the adaptation process. Her team held twice-daily huddles at 8 a.m. and 8 p.m., often for just 15 minutes, to talk about what happened during the day, discuss any glitches and brainstorm solutions, and disseminate any new solutions or adaptations. These debriefs were important for not only implementing PATCH-24 but also connecting with physicians in different hos-
pitals. She noted that the overall amount of meeting time has diminished since then, and she and many of her colleagues miss meeting so frequently.
PATCH-24 relied heavily on physicians because they were available; chaplains and social workers were consumed with their expanded roles on the palliative care consult teams embedded in ICUs. Ankuda believes that incorporating the full interdisciplinary team in such programs would be extremely useful, particularly if patients and families were screened in advance to identify who would benefit most from interdisciplinary team care. She noted that even if the entire team could not join every call, having sequential communication among the full team would likely benefit patients. In closing, Ankuda shared that one problem she worried about initially did not come to fruition: that ED staff would continue calling on her team at all hours of the day after the COVID-19 surge abated. “We found that was not a problem at all,” said Ankuda. “Everyone understood that we were all acting outside of our normal workflow.”
A Clinical Chaplain’s Perspective
Kristopher Halsey, a clinical chaplain and bereavement support specialist in Philadelphia, PA, explained that at the time of the initial COVID-19 outbreak, he was working as a chaplain for a local hospital, but at the time of the workshop was working as a hospice specialist. He pointed out the significant challenges of supporting patients, families, and staff given pandemic restrictions. For example, the lockdown of long-term care facilities made it extremely difficult to provide hospice services that would support the end-of-life needs of both patients and family members. Personally, Halsey experienced the weight of what families were dealing with when his aunt, who lived in a long-term care facility, developed COVID-19 and passed away. “Closure was not there, which led to what is now labeled as pandemic grief,” he said.
Halsey recalled when he was working in the hospital and one of the ICU patients died of COVID-19, the ICU nurse had to bring the body to the hospital morgue. Seeing the the bodies of all the other people was traumatizing for her. Halsey received a call at 9 p.m. to meet with the nurse to try to help her deal with those painful emotions.
Halsey also recounted how the hospital passed out Chromebooks to patients so that he could deliver Sunday services virtually and provide spiritual care and support. Patients were still struggling, however, because they could not receive the one-on-one, in-person care they needed. In addition
to supporting patients, Halsey added, he and his fellow chaplains ministered to staff, instituted partnerships with the local Department of Health to provide testing for the community, and helped churches and faith leaders continue to provide support to their congregations.
One lesson Halsey learned was the importance of working together in times of crisis and respecting one another’s roles in providing support. Halsey observed that it was equally important to reinforce the message that staff needed to take care of themselves along with their patients. Wellness debriefings were one way to provide virtual support to both staff and patients.
In closing, Halsey pointed to the need to be present for people even after the pandemic. “Studies have shown there will be a bereavement crisis that is going to come on,” he said. Given this looming crisis, continuing to partner across disciplines will become even more important.
Bellevue and NYC Health + Hospitals’ Response to the Patient Surge
To put her institution’s experience during the pandemic’s early days in context, Susan Cohen, medical director of the palliative care program at NYC Health + Hospitals/Bellevue, noted that Bellevue is the nation’s oldest public hospital. It is part of an 11-hospital, 5-nursing-home system that makes up the largest U.S. safety net system. Bellevue has a history of responding to pandemics, epidemics, and large-scale disasters dating back to the days of yellow fever, cholera, small pox, and tuberculosis and continuing through the HIV/AIDS epidemic, hurricane Sandy, and the outbreak of the Ebola virus. She also pointed out that many of Bellevue’s patients have histories of trauma, poor access to care, and cultural and linguistic barriers.
Cohen emphasized the importance of remembering the fear and emotion that hospital staff experienced in the spring of 2020. PPE was in short supply, and staff were concerned the hospital would run out. Tests took 4–5 days to produce results and were only available for hospitalized patients. Hospital mask mandates did not exist until May 2020, when the surge was already waning, and staff only wore masks when entering rooms of patients with suspected or confirmed COVID-19, to ration PPE. Cohen recalled how she had to walk past a dozen refrigerated trucks every day, which served as makeshift morgues and represented just one of the many facets of the trauma she and the rest of staff were experiencing.
Cohen explained that when she thinks about pandemic planning and preparedness, she uses a tsunami analogy; people in the know recognize that water recedes far into the ocean before the tsunami hits land. “That is how I felt during the preparation stages,” she said. “I knew what was coming, and
I was really panicking about what we could do.” To prepare, Cohen spoke to colleagues in Seattle, where the first COVID-19 wave struck. In the end, she went with a learning-by-doing approach, because while planning and preparedness were helpful, she had to be adaptable when the reality of the pandemic struck New York.
As Cohen and her colleagues were upscaling their ability to care for patients from a palliative care perspective, they decided that they would ensure that staff had real-time information when communicating with family members. “We heard of a story where someone got an update and a death call within minutes of each other because the information that the caller was using was not accurate and up to date in real time,” said Cohen. To prevent that, the palliative care team embedded itself in the ICU and paired up with the ICU teams, which established solid, relational communication. They only made calls after contacting the ICU. “We did utilize telehealth, but we felt that in-person, embedded practice made a huge difference for our patients,” said Cohen.
By incorporating in-person volunteers, Cohen could increase capacity rapidly from one team to three teams. The volunteers—most from child and adolescent psychiatry and community-based psychiatry practices—received brief trainings using materials from the Center to Advance Palliative Care and VitalTalk.12 Her institution also mentored the volunteers by having them work closely with a team that included one of her unit’s experienced practitioners. During the first wave, her unit’s patient census increased fourfold, and fellows took on leadership roles because it had only two palliative care providers and an internist. Despite the limited supply of palliative care clinicians, coverage increased to 7 days a week for 5–6 weeks.
Palliative care team members’ roles included providing medical updates to family members, supporting care teams through ethical issues, and engaging in care planning and discussions of patient goals and values. Since many of the patients were young and previously healthy, the palliative care teams also had many discussions about life-sustaining treatments. While providing support for care teams, Cohen was mindful of her own teams’ wellness. “Fortunately, our wellness work had already started the year prior,” she said, adding that she enlisted a wellness coordinator who had worked with her team to conduct sessions every other week during the COVID-19 surge. Her team also took advantage of Bellevue’s existing Helping Healers Heal program,13 respite rooms, and other wellness activities.
___________________
12 See https://www.vitaltalk.org (accessed March 10, 2022).
13 See https://www.nychealthandhospitals.org/pressrelease/employee-wellness-program-to-address-emotional-stress-and-burnout (accessed June 8, 2022).
Cohen pointed to the importance of remembering that each team member has a different trajectory for their fear, grief, anger, and gratitude. She also noted that the tragedy of George Floyd’s murder came right after the surge, had a huge impact on her team, their patients, and the health system, and served as a repeat trauma that further affected the team’s wellness. In closing, Cohen noted that the history and culture of Bellevue and NYC Health + Hospitals helped prepare staff for the surge. The ability to adapt and her team’s prior wellness and resilience work was critical to dealing with it.
Focus on Health Equity
L. Ebony Boulware, chief of the division of general internal medicine at Duke University School of Medicine, began by stating that “the inequity story is the pandemic story,” given that individuals from historically underserved communities shouldered much more of the brunt of the COVID-19 pandemic (see Figures 2 and 3). COVID-19 hospitalization and death rates, she noted, were 4–6 times higher in Black/African American and Hispanic/Latinx communities compared to other communities (Li et al., 2020). In addition to tremendously negative health effects, these same communities were experiencing loss of jobs and health insurance, economic instability, mental health effects, and structural barriers to health care. In short, the pandemic exacerbated underlying weaknesses in these communities.
In addition, the pandemic had a more severe economic impact on underserved and historically disadvantaged communities, as they were more likely to work in vulnerable jobs or in positions on the frontlines of the pandemic with little workplace protections against exposure to the virus, explained Boulware. While job loss affected all communities, there was a large racial inequity in loss of employment (see Figure 4) (Saenz and Sparks, 2020). This exacerbated disparities given the link between employment and health insurance coverage. The combination of loss of health insurance and economic instability meant that many Black/African American and Hispanic/Latinx individuals were 1.5- to 2-fold more likely to delay or avoid urgent or emergency care compared to white individuals. Those delays, said Boulware, often resulted in negative health consequences.14 In
___________________
14 See https://www.rwjf.org/en/library/research/2020/09/the-impact-of-coronavirus-on-households-across-america.html#:~:text=While%20billions%20of%20dollars%20have,not%20been%20protected%20from%20serious (accessed March 15, 2022).
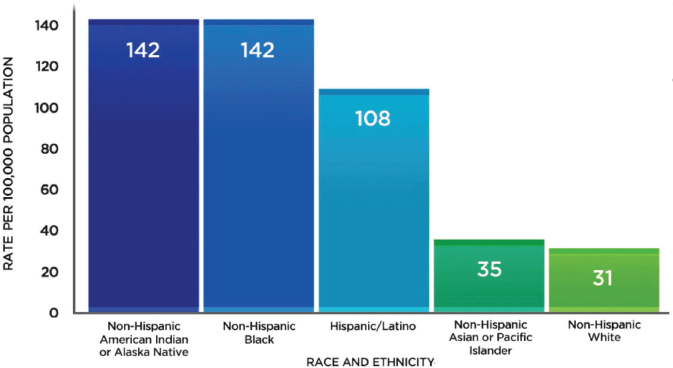
SOURCE: As presented by L. Ebony Boulware, November 8, 2021; content adapted from CDC, 2021. Data Visualization. https://www.cdc.gov/coronavirus/2019-ncov/covid-data/data-visualization.htm (accessed June 8, 2022).
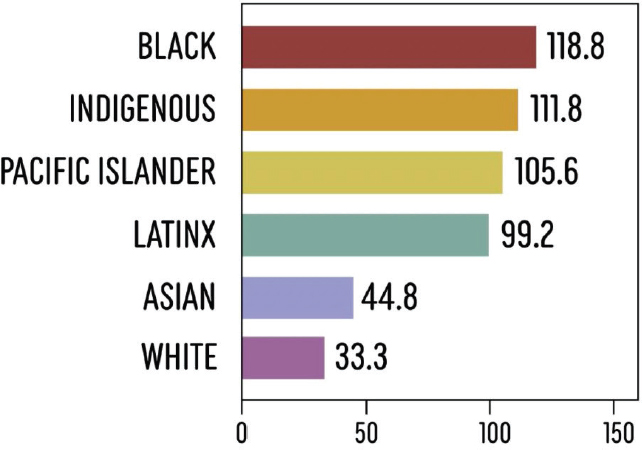
SOURCE: As presented by L. Ebony Boulware, November 8, 2021; Li et al., 2020.
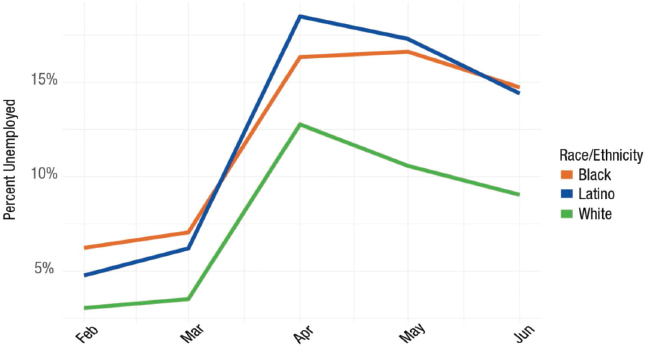
SOURCE: Presented by L. Ebony Boulware on November 8, 2021; content adapted from Saenz and Sparks, 2020. https://carsey.unh.edu/publication/inequities-job-loss-recovery-amid-COVID-pandemic (accessed June 8, 2022).
addition, individuals in Black/African American and Hispanic/Latinx communities experienced more stress, anxiety, and great sadness that they found difficult to cope with, as did women compared to men and all individuals with below-average income compared to those with above-average income.
Boulware pointed to the increased use of alternative methods of connection, primarily telehealth, as one bright spot during the pandemic. She noted that one study found that Black/African American and Hispanic/Latinx individuals were more likely to report using telehealth to connect with physicians or other medical professionals (Campos-Castillo and Anthony, 2021). However, two studies found that timely access to care was a key contributor to inequitable outcomes during the pandemic (Price-Haywood et al., 2020; Yehia et al., 2020), with Black/African American individuals more likely to present sicker than white individuals. Boulware offered several reasons people may have delayed care, including workplace conditions, structural barriers such as difficulty arranging transportation, and economic barriers. Once people were in the hospital, race was not associated with prevalence of in-hospital death. “They show up sicker, but once they have access to care, it appears that inequities could be mitigated,” Boulware explained, while emphasizing that inequity in access to care “is a key contributor to the inequities in the outcomes.”
Describing how COVID-19 inequities changed over time, Boulware pointed out that in the initial phases of the pandemic, Black and Hispanic/-
Latinx individuals had higher rates of morbidity and mortality (Figure 5). By June of 2021, however, Native American, Alaska Native, and Indigenous individuals were experiencing much greater inequities than other groups. “We cannot always think that what we saw in the beginning is the pattern that is happening over time,” she said. “These patterns are changing and continue to change, and we need to monitor and focus on the groups experiencing inequities at the time.”
“I think the pandemic clearly brings out the weaknesses in our health care safety net and our societal factors that can lead to health inequities,” observed Boulware. She emphasized that a lesson learned from the pandemic is the need to go beyond a focus on medical needs, to “the nonmedical determinants—housing, employment, and the rest of our social safety net—to deal with inequities. … At the end of the day, what has become clear is that the answers cannot come just from within the health care and public health sectors. They need to come from across multiple sectors of society to address these inequities,” Boulware concluded.
Discussion Session
Lori Bishop, vice president of palliative and advanced care at the National Hospice and Palliative Care Organization, and Karen Bullock, professor and John A. Hartford Scholar at North Carolina State University, co-moderated the discussion session. Bishop asked the speakers about the
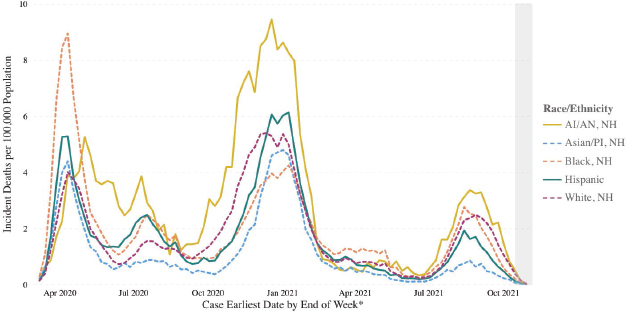
SOURCE: As presented by L. Ebony Boulware, November 8, 2021; content adapted from CDC, 2022. https://covid.cdc.gov/covid-data-tracker/#demographicsovertime (accessed June 8, 2022).
state of the partnerships and innovations they developed during the initial phases of the pandemic. Davis replied that during the height of the pandemic, health systems across all 16 of the markets in which her organization operates—not just the hospital where she opened the inpatient unit—began to appreciate the innovation and responsiveness, as well as the value proposition of hospice and palliative care. She added that the hospital in which the hospice inpatient unit was created shared with her that it was thrilled about the partnership that developed and would like to continue it. Davis noted that she would like to see research on the factors that led to the highly variable acceptance of hospice across markets.
Cohen emphasized that the relationships her team built with the health system’s ICUs were critical to being able to create and upscale her program. At the onset of the pandemic, the ICU units were too busy to reach out, but because of preexisting relationships, ICU staff embraced her team. Ankuda agreed that preexisting relationships with EDs made it much easier to introduce PATCH-24 than with EDs that had not previously bought into palliative care. She noted that a colleague conducted an informal survey of ED physicians at the end of 2019 to see if they thought palliative care was part of their job, and the majority said no. When this colleague resurveyed ED physicians after the pandemic began, the majority said yes.
Bullock, referring to Carrol’s earlier presentation and reflecting on Halsey’s comments, asked Halsey if the concept of hope and healing resonates with him based on his experiences. Halsey replied that hope and healing are huge, in large part because of the lingering uncertainty about infections, vaccinations, and boosters. Halsey noted that he has learned to continue to offer hope to patients and families. He reminds them that they have to do what is best for them but also discusses, for example, the possible ramifications of not being vaccinated. He collaborates with clinicians to provide educational opportunities for families and provides virtual talks at his local church to help educate that community about the importance of widespread vaccination to enable the community and the nation to move past the pandemic. Regarding what he does when he needs support, Halsey said he turns to another colleague to debrief and have someone who engages in nonjudgmental listening. He also tries to use the tools he encourages others to use, such as encouraging people to engage intentionally in a favorite hobby.
In response to a question about the greatest challenges to addressing the determinants of inequities, Boulware pointed out that it is necessary to start thinking about the arc of health care in terms of everything that is
required in order for an individual to show up and be able to get what they need out of the health care system. This will require addressing structural, economic, and other barriers to accessing services in the health care system and partnerships that go beyond the current public health infrastructure to include community-based organizations and government agencies. Bullock added that she often hears colleagues say, “if we build it, they will come,” but often-inadequate transportation options or cultural or spiritual issues serve as barriers.
Bishop, posing a question from a participant, asked how the health care system could address the enormous amount of workplace stress and frustration that has built up during the pandemic beyond encouraging self-care. Cohen said that for too long, the responsibility for self-care fell solely on providers, but we now realize that health care systems need to build more resilience and wellness into their operations that goes beyond having a quiet room or providing a voucher for a massage once a month. Cohen said that research is needed because the health care system is already facing another crisis: getting people to enter the workforce, stay in it, and be able to function well in the system without being angry, irritable, burned out, and disengaged.
Ankuda said that one thing she noticed throughout the pandemic was the extraordinary camaraderie and sense of spirit among staff. Some of that, she suspected, was that staff had more energy and thought that the situation would be over soon. However, she wondered if some of it also was the result of greater freedom to innovate and less paperwork and regulatory burden to shoulder. “We were all working at the top of our license, and we were all driven by intense meaning in what we were doing,” she said, sentiments with which both Cohen and Davis agreed.
As much as the health care system needs to address clinician wellness issues, Ankuda suggested that it also needs to address staff’s struggles with paperwork, electronic health records, and other bureaucratic responsibilities that have increased over the years. She also noted the gender inequalities that the pandemic highlighted in terms of caregiving responsibilities and hoped that health system leadership would address this issue.
Bishop asked the panelists to talk about what they have learned regarding any new expectations that employers might have. Cohen said that the leaders of her facility appreciated the camaraderie and spirit of teamwork that developed during the initial stages of the pandemic as well as the innovative approaches developed by staff members. She was uncertain whether and how leaders will act to sustain those positive developments in more
normal times, and she expressed concern as to whether health system leaders will address staff’s long-term mental health issues. Her hope was that the lessons learned from crisis management and about inequities will inform decisions made by health system leaders in the future.
Boulware noted that it remains to be seen if employers will provide protections for people who suffer lasting effects, known as “long COVID.” Because of the inequities in how the pandemic has played out, she suspects that individuals from historically underserved groups are going to be further disadvantaged by a lack of workplace protections related to long COVID. She called for efforts to promote actions that would support and protect people as they continue to experience the full impact of the pandemic.
As a final question, Bullock asked Cohen to elaborate on the trauma of staff she referenced in her presentation. Cohen replied that what she noticed in herself and her team members was that everyone had a unique way of coping with the anxiety related to concern about their health and that of their families. Even palliative care clinicians, social workers, and chaplains who deal with death and dying found themselves unprepared. Referring to the sheer volume of patient deaths, she pointed out, “This is not normal, not in health care, not anywhere, and it was traumatizing.” Cohen described how some staff members were panicked and refused to come to work in the early days of the pandemic, others needed to take time away for their own mental health when the initial surge ended, and still others are now just working through their trauma.
Cohen shared that her palliative care team realized that the ICU was filled with Hispanic/Latino men whose family members were actually in the same ICU. The families were traumatized, and members of her team were stunned by the multiple losses families were experiencing. All the things palliative care staff normally deal with were amplified significantly, Cohen observed, which raises the critical issue of how the health care system will care for its workers because that type of profound trauma does not just go away.
Closing Comments from the First Webinar
Bowman closed out the first webinar by reflecting on what she heard during the sessions. The fear, uncertainty, and chaos of the pandemic’s early days stood out for her, as did the power of teams motivated by love, vocation, and camaraderie to pull off incredible feats. She recalled the les-
sons learned about what it takes to navigate uncertainty and be resilient as a health system, as teams, and as individuals; how to learn and iterate; and how crucial strong leadership is to enabling that to happen. Bowman also noted how the quick innovation of palliative care and hospice teams made a meaningful difference in the experiences of patients with COVID-19 and their families and how critical it was to their health care organization’s ability to meet the moment.
The speakers highlighted the preexisting gaps in care for patients with serious illness, which were exacerbated by the pandemic, said Bowman. Chief among these were the glaring disparities in the experiences and outcomes of Black and Brown communities. She noted that the third webinar in this series would aim to synthesize promising opportunities to address these gaps in high-quality serious illness care. She concluded her summary by previewing the two topics that the second webinar would address: telehealth and the health care workforce.
The key themes that Wang took away from the first session’s presentations included Fineberg’s discussions of how leadership, science, public trust, preparedness, and strategic response are required for recovery and Carrol’s acronym for change as a constant. The first session highlighted key issues, including the value of team-based care, the need for interprofessional training, the critical role of palliative care as a specialty as well as a skill set for all clinicians, and how virtual platforms helped provide patient-centered care. The session also emphasized the importance of addressing health inequities and deficiencies by increasing attention to the social determinants of health.
In summarizing the key takeaways of the second session, Wang noted that it described several examples of remarkable innovations and the critical role that safety net hospitals serve in the community. She emphasized that “adaptability to crisis demands interdependence of health systems and departments. Routine communication, telehealth, community engagement, creative staffing, intentional inclusion of non-physician team members, [and] hospital partnerships with public health and places of worship” are all beneficial tools to improve care for patients with serious illness, particularly during a crisis.
WEBINAR TWO
Bowman opened the second webinar in the series with a brief recap of the first webinar and its focus on the innovative responses in the initial
stages of the pandemic. She also noted that the first webinar included discussions about health equity and referred back to Boulware’s comment that the story of the pandemic is also the story about inequity.
Workforce Challenges and Innovations
Bowman explained that the second webinar in the series would focus on the workforce that cares for people with serious illness and telehealth. These two topics, she pointed out, are inextricably linked. During the pandemic, many health systems nationwide were able to use telehealth to extend the reach of a scarce resource, their palliative care teams. Technology also enabled families to connect with loved ones, and the capacity to make those connections helped relieve some of the moral distress that the battered health care workforce was experiencing.
The Lived Experience
Rodney Tucker, director of the University of Alabama at Birmingham Center for Palliative and Supportive Care, opened the second webinar by sharing his lived experience during the pandemic. Beginning in March 2020, he explained, almost everyone was doing everything “right” by shutting down, working remotely, exercising proper hygiene, and wearing masks. From July to December 2020, people largely continued to do everything “right” and were looking forward to a better 2021 with vaccines on the horizon. The vaccines arrived in January 2021, along with the worst surge in COVID-19 cases in Alabama. Though fatigued, people largely continued to do the “right” thing, but by April and May of 2021, people let their guard down slightly, and Tucker became frustrated with the lagging vaccination rate.
Tucker shared that in June, despite being vaccinated, he tested positive for the Delta variant and his spouse developed bilateral pneumonia. Noting that this served as a serious test of his empathy, he shared a diagram to illustrate his emotional trajectory during this time (see Figure 6) and said he was at the “anniversary reactions” stage with the impact of the Delta variant on his family.
Tucker identified several challenges he and his team felt, both professionally and personally (see Figure 7). These contributed to diminished resiliency and burnout. In looking for measures to reinforce resilience and prevent burnout, Tucker and his team measured their well-being index
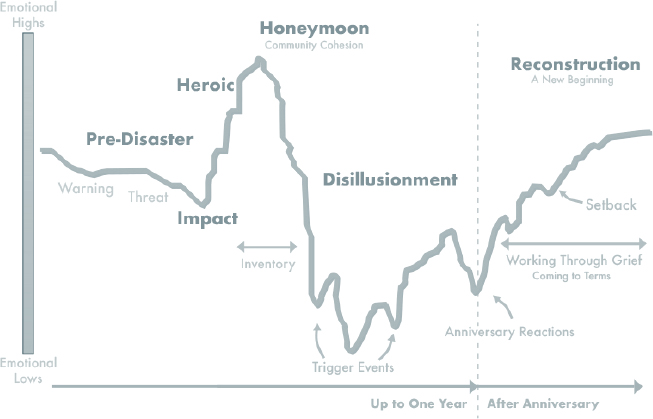
SOURCE: As presented by Rodney Tucker, November 18, 2021; adapted from Dewolfe, 2000.
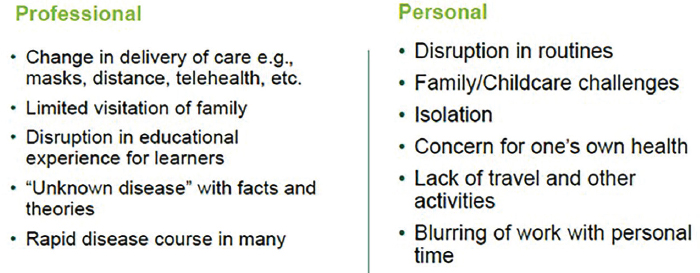
SOURCE: As presented by Rodney Tucker, November 18, 2021.
to understand the trajectory of their response during this period. Tucker shared that he encouraged team members to take three simple actions: (1) be flexible in terms of scheduling and being able to help one another; (2) take advantage of the power of the debrief, which is something practiced in palliative care; and (3) have “grace in their sails.”
Tucker explained that his team began applying practices associated with the “Circle Up” framework, which uses briefings, micro check-ins, and debriefs to strengthen resilience, sustain psychological health, and maintain care excellence (Rock et al., 2020). Tucker noted that using these practices to check in, be heard, and listen to one another helped the team work well together. Team members also checked in with each other about how their work affected them personally and made sure they were feeling all right before they went home. “This seems to be something that we all appreciate and that helps us to regain some of our energy, some of our resilience, and to know that we will be okay, one step at a time, one debrief at a time, one conversation at a time as we all strive to look to see what is our next normal,” explained Tucker. The power of Circle Up, he added, is that it helps him and his teammates deal with the uncertainty about the future, and what the next normal would look like.
Tucker concluded by sharing a poem he wrote together with his “poet listener.”15 Titled Farewell 2020, the poem is an emotional reflection on his lived experience caring for people with serious illness throughout the pandemic.
Farewell 2020
2020: You’re coming to a close with
Contradiction
Disruption
One-dimensionality,
Life-changing chaos,
Prolonged paradox,
Invigoration and frustration,
Gratefulness and fearfulness.
2020: You’re coming to a close, and
I still don’t like yoga.
I meditate to pop (Latin dance) music.
___________________
15 See https://www.goodlistening.org/programs/listener-poets (accessed March 10, 2022).
I still hate podcasts and binge on Netflix.
I show grace to myself in how I find resilience;
There is no one way that works for everybody.
I don’t tell others how to find it.
I don’t want others telling me.
2020: You can’t come to a close fast enough.
You left me not knowing how to feel or act.
You’ve challenged the can-do side of me.
You’ve got me questioning what I’ll feel looking back.
Will I be sad about what was taken away,
Or happy to have come through, healthy?
2021: For you, I have one intention –Simply stay well and sane.
COVID-19 and the Nursing Workforce
Elaine Larson, the Anna C. Maxwell Professor of Research Emerita and Special Lecturer at the Mailman School of Public Health at Columbia University and Senior Scholar in Residence at the New York Academy of Medicine, discussed how the pandemic has affected nurses, particularly those working with individuals with serious illness who receive home care or are in long-term care facilities. She pointed out that nursing is the nation’s largest health care profession, with nearly 4 million registered nurses (RNs) nationwide, according to the American Association of Colleges of Nursing (AACN).16 Nevertheless, even prior to the pandemic, shortages of registered nurses were projected through 2030 (Zhang et al., 2018). Changing U.S. demographics—an aging population and a higher prevalence of serious, chronic illness—are driving the demand for nurses at the same time that a considerable proportion of the nursing workforce is nearing retirement, stress and job dissatisfaction are on the rise, and burnout has been exacerbated by the pandemic (AACN, 2020). These workforce pressures are occurring against the backdrop of research that indicates “a significant correlation between inadequate nurse staffing and higher rates of adverse events, morbidity, and mortality,” Larson pointed out (Aiken et al., 2014; Kane et al., 2007; Shekelle, 2013).
Larson referred to a 2020 survey that found that 22 percent of nurses surveyed indicated they may leave their current positions, and 60 percent
___________________
16 See https://www.aacnnursing.org/news-information/fact-sheets/nursing-shortage (accessed March 10, 2022).
of that group said they were more likely to leave given the added stress of the pandemic.17 Nurses cited insufficient staffing, unsafe workload, and the emotional toll of the pandemic as key reasons for wanting to leave. Other workforce-related problems identified were regional variations and shortages, specialized skill gaps, and the need for strategic workforce planning. “Hence, as with inequities in patient access and care, problems with nursing workforce are long-standing and embedded in the system, but COVID exacerbated and highlighted existing conditions,” said Larson.
Turning to seriously ill people who are in long-term care or home care settings, Larson said that even prior to the pandemic, infection was a primary cause of morbidity and mortality in long-term care settings. As an example of an infection mitigation effort, Larson discussed the COVID-19 Action Network18 that the Extension for Community Healthcare (ECHO) project at the University of New Mexico launched in September 2020. Project ECHO, uses a hub-and-spoke, telementoring, knowledge-sharing approach in which expert teams lead virtual clinics to reduce disparities in underserved and remote communities (Katzman et al., 2021). Larson explained that approximately 9,000 nursing homes participated in 16 weekly sessions that included short lectures, case-based presentations, the development of quality improvement skills, and group discussion. The New York Academy of Medicine’s training center, for example, recruited, planned, and convened weekly sessions for approximately 150 nursing homes in New York and Connecticut.
Larson shared some findings from qualitative interviews with a number of nursing homes in the metropolitan New York area, which revealed that frontline caregivers, primarily certified nursing assistants, are often people of color and/or first generation immigrants with little formal training and who are paid minimum wage. Larson said that many hold several jobs to support their families, increasing the risk of cross transmission between facilities and reducing job satisfaction and staff retention. She added that while improved training is associated with enhanced infection control practices, staff responsible for infection control tend to have little training in infection control and have multiple responsibilities.
In closing, Larson offered four ways to support the nursing workforce:
___________________
17 See https://www.trustedhealth.com/the-handoff-podcast/joanne-spetz (accessed March 10, 2022).
18 See https://www.ahrq.gov/nursing-home/index.html (accessed March 10, 2022).
- Make workforce health and well-being part of the system by providing equitable and adequate wages; recognition, appreciation, and economic rewards commensurate with value; resources for staff mental health and work breaks; and transparent communication to frontline direct care staff.
- Increase workforce flexibility, require less overtime, and enhance staff and patient participation in decision making and scheduling.
- Reimagine delivery models and improve organizational climate by leveraging digital tools, adapting care models based on patient and employee preferences, supporting leadership training programs and mentorships, and building learning networks and coalitions across agencies and systems of care.
- Strengthen talent pipelines and build skills for the future by implementing national training requirements for frontline staff based on core competency standards, supporting reskilling when needed, and bolstering recruitment pipelines for clinical roles.
In particular, Larson stressed the need to support leadership training programs and mentorship given the strong correlation between leadership, and job satisfaction and staff retention. In closing, she acknowledged that implementing these four improvement approaches would require major change in the structure of the nation’s acute and chronic care systems.
Hospice and Home- and Community-Based Care in the Pandemic
Liz Fowler, president and chief executive officer of Bluegrass Care Navigators, opened by noting that her organization is a Joint-Commission-accredited provider of hospice and home- and community-based services, including home-based primary care, for thousands of frail and seriously ill individuals each year. Bluegrass Care Navigators, headquartered in Lexington, KY, has 750 team members operating out of seven regional offices serving both urban and rural communities throughout the state. Some of its clients live in counties with the highest poverty levels in the nation, and some even live in homes that lack adequate electricity or clean water.
Fowler noted that Kentucky was spared the initial waves of the pandemic, but she and the rest of the staff were watching what was happening in Oregon, New York, and other parts of the country. Her colleagues shared stories of closing entire inpatient hospice units or losing much of their team to the pandemic and illness. “We were scared, and some panic was setting
in,” said Fowler. The organization’s response was to establish a communication process that was disciplined and thoughtful. For example, headquarters sent out a standardized daily e-mail at 5:30 a.m. using the Situation, Background, Assessment, and Recommendation format (Leonard et al., 2004).19 This system ultimately served the organization well.
Fowler and her colleagues also took a close look at the available workforce to get an idea of how the teams would care for patients if team members became ill or unavailable. They developed plans for each team member’s role and decided which services the teams would provide under contingency, crisis, and catastrophic staffing levels. Fowler explained that the organization cross-trained everyone for alternate jobs. Nurses in administrative roles were trained to conduct home visits, for example, and office staff were trained to serve as medical equipment technicians who could decontaminate equipment and subsequently install it in clients’ homes. The teams knew who would come to perform what services under contingency levels compared to crisis levels. Fowler noted that while they never reached catastrophic staffing levels, the organization was prepared for that eventuality.
Building on Tucker’s remarks, Fowler explained that she realized that the organization had to provide a great deal of personal and professional support to its workers. When Kentucky declared a state of emergency and everyone transitioned to remote work, Fowler concluded that team members needed flexibility, given that schools were closed and other services were unavailable. It was fortunate, she said, that her organization could provide care at any time of the day as long as staff communicated with the regional offices. Managers, said Tucker, “leaned in” to what their individual team members needed, and the organization surveyed members regularly to identify their needs rather than assume. For example, the organization initially proposed an on-demand tutoring system to relieve challenges in homeschooling children. However, when management surveyed team members, they learned that the team was more concerned about not having desks and laptops at home. The organization opened its offices to allow team members to pick up desks as well as refurbished laptops for use at home. Fowler noted that Bluegrass Care Navigators’ core values of compassion, respect, and dignity served the organization, team members, and clients well. “We did what we needed to do for our team members to show them compassion, to show them respect, to show them dignity,” said Fowler.
___________________
19 A detailed tool is available at http://www.ihi.org/resources/Pages/Tools/SBARToolkit.aspx (accessed March 10, 2022).
Bluegrass Care Navigators also hired coaches to help the organization’s managers normalize their sadness, exasperation, and fatigue. They circulated the Professional Quality of Life Scale20 instrument to all team members and discovered that 70 percent felt worn out by their work and 64 percent felt overwhelmed by their work assignments and felt that their work was never ending (Stamm, 2009, 2010). “We knew something was going on and more needed to be done for our team, but this really was startling to us,” said Fowler.
Fowler explained that Bluegrass Care Navigators, which is self-insured, simultaneously began to see a staggering increase in health care claims for short inpatient stays. Depression ranked fourth in diagnosed chronic conditions among staff claims—approximately 50 percent higher than the benchmark—and attention deficit hyperactivity disorder ranked seventh. The organization responded to the team’s needs by having a clinical psychologist conduct mindfulness moments for which any team member could call in at any time. Bluegrass Care Navigators also partnered with the Schwartz Center for Compassionate Health Care to offer Schwartz Rounds,21 which create a safe place for team members to work through their feelings and normalize and process their roles as caregivers for people with serious illness.
Fowler explained that in May 2021, the organization implemented a mental health normalization campaign for its workforce that had two components. The first component, similar to the Heart of Hospice approach discussed in the first webinar, consisted of a Code Lavender response team to provide the teams with debriefings for stressful work-related incidents (Stone, 2018). Any team member could request one, and peers could even do so for other team members. The second component, designed to support the workforce, was a compassionate leave policy created with the help of frontline team members. Similar to family medical leave, it enables someone to request up to 12 weeks of leave that they can use intermittently or in blocks of time. Team members can use paid time off, time from a sick leave reserve bank the organization established, or unpaid time off to recover, rejuvenate, process, and deal with their grief. In addition, staff meetings include a mindfulness moment, and business meetings include asking staff how they are feeling. The organization has even been teaching meditation
___________________
20 The Professional Quality of Life (ProQOL) scale is one of the most common questionnaires used to measure burnout, compassion fatigue, etc. among health care professionals.
21 See https://www.theschwartzcenter.org/programs/schwartz-rounds (accessed March 10, 2022).
and other techniques that can help individuals reset. “We are hoping that all of these things will help us be more sustainable, reduce our absenteeism, engage our workforce, and improve productivity,” said Fowler.
Fowler pointed out that the organization established a 24/7 call center that team members and their families can call into for support. It has also expanded its use of nonlicensed team members, including scribes and CHWs, and developed partnerships with other providers, such as emergency medical services and medical equipment companies, to reduce the burden on staff.
In closing, Fowler pointed out the legislative and regulatory work needed at the state level to allow the organization to make more use of unlicensed workers or those licensed for other tasks. For example, paramedics must work under the direction of an emergency medical physician or emergency medical director, so regulatory and legislative changes may be necessary to integrate them more effectively into the workforce caring for people with serious illness.
The Role of Community Health Workers in the Pandemic
Shreya Kangovi, founder and executive director of the Penn Center for Community Health Workers and associate professor at the Perelman School of Medicine, opened her remarks by reinforcing what previous speakers had highlighted: the pandemic has had a disproportionate impact on people of color and people living in rural areas. “These are the people in our hardest-hit communities in America who have been seriously ill, who have been dying at startling rates, not only of COVID and its effects, including deferred preventive care and mental health challenges, but also due to long-standing issues such as food insecurity, police violence, and disparities of every kind,” she explained.
Kangovi explained that in her view, health inequity is “a psychological condition that affects those of us who are privileged. It is psychological because it takes such forms as racism, group narcissism, xenophobia, and savior thinking… and those are psychological distortions.” Those distortions then make their way into policies, whether for federal housing, Medicaid coverage, clinic no-shows, or institutional hiring. Those policies shape the distribution of wealth and power across the nation’s institutions and society in a manner that has an impact on living conditions and social needs, which affects behaviors and health across different domains, Kangovi observed.
“When we think about health inequity that way, I think it challenges us because we tend to have conversations about health inequity that are quite ‘othering,’ where people who are privileged talk about how can we help and fix those people who face inequities,” observed Kangovi. A transfer of power is required to improve health inequity in Kangovi’s view, because “it is not enough to just address unmet social needs or navigate people, even with the best of intentions.”
Kangovi pointed out that community-based organizations have long hired CHWs to provide a range of social support, advocacy, coaching, and navigation to people in their communities as a means of improving their health. CHWs, explained Kangovi, share life experiences and come from the same communities as the people they serve.22 They are a diverse reflection of the U.S. communities hardest hit by the pandemic: 65 percent of them are Black/African American or Hispanic/Latinx, 23 percent are white and often in rural or low-income communities, and 10 percent are Native American.23 “They may not have extensive formal schooling, but they do have lived expertise of racism, of injustice, of financial hardship,” she said.
Kangovi explained that health programs using best practices select CHWs based on personality attributes, such as being empathetic, altruistic, and nonjudgmental.24 These attributes are critical to their work; rather than merely compiling a list of social needs, for example, CHWs tend to “listen to people, they get to know their life stories,” said Kangovi. CHWs find out who people are and what they think they need to live their best lives and then work to deliver those things. In Kangovi’s view, CHWs are the “power grid, not the lampposts.”
Observing that CHWs do not think in terms of disease or domain silos but rather work across domains and conditions, Kangovi explained that this capacity gives them power, as does their ability to intervene at all stages of the health inequity trajectory. CHWs are able to navigate access to care and bridge gaps with health teams to improve health outcomes, while also provide coaching about healthy behaviors and address unmet social needs. “By definition, if we transfer power to community health workers, we are
___________________
22 See https://www.nachc.org/wp-content/uploads/2020/01/Chartbook-2020-Final.pdf (accessed March 10, 2022).
23 See http://www.institutephi.org/wp-content/uploads/2014/08/survey-of-Community-Health-Workers.pdf (accessed March 10, 2022).
24 See https://www.ncqa.org/wp-content/uploads/2021/11/Critical-Inputs-for-Successful-CHW-Programs-White-Paper-November2021.pdf (accessed March 10, 2022).
reshaping the distribution of wealth and power in our institutions and within health care and public health more broadly,” said Kangovi.
Kangovi also pointed out that CHWs have policy expertise derived from lived experience. Who better, asked Kangovi, to redesign the Supplemental Nutrition Assistance Program, for example, than someone who has firsthand experience at the checkout counter? In addition, CHWs are starting to lead antiracism and social justice innovations. At Penn Medicine, Kangovi explained, the chief executive officer and other senior executives now have CHW mentors who train them on what it is like to live with some of these inequities (Vasan et al., 2021).
Kangovi noted that CHWs are one of the most evidence-based workforces in health care and public health. For example, multiple randomized, controlled trials have demonstrated that they can move the needle on chronic disease control, cancer screening, access to and quality of care, and reductions in hospitalization (Kangovi et al., 2018; Vasan et al., 2020). Moreover, research suggests that they can save approximately $4,200 per Medicaid beneficiary, a $2.50 return on investment for every dollar invested in a CHW program (Kangovi et al., 2020).
To identify the factors that produce these positive outcomes, Kangovi conducted approximately 1,500 interviews with patients at their bedsides, on porches, and in shelters, asking them what makes it hard for them to stay healthy and what CHWs should be doing differently when designing programs. She and her colleagues also studied other CHW programs to gain insights into what worked and what did not. The result was Individualized Management for Patient-Centered Targets (IMPaCT), a standardized, scalable program that leverages CHWs to improve health and address certain historical challenges these programs have faced (Kangovi et al., 2018, 2020; Vasan et al., 2020).
Turnover, for example, has been a perennial challenge, so she and her colleagues developed hiring toolkits that allow programs to select trustworthy individuals with shared life experiences. IMPaCT produces playbooks and infrastructure that enables CHWs to have a person-centered work practice, where they can get to know people’s life stories and improve their lives. The program also provides compensation and supervision that is supportive and relies on supervisors who understand how to work with CHWs. “All of these elements are critical, and, on a programmatic level, have allowed us to build out this program and replicate it across 20 different states,” said Kangovi. She noted that during the pandemic, co-designing with frontline
workers was critical to ensuring that they participated in health care decision making, design, and delivery.
Kangovi identified standards and financing as the two components for successful scaling of these programs. Over the past year, she explained, her team has collaborated with the National Committee for Quality Assurance (NCQA), the National Association of Community Health Workers, and other stakeholder organizations across the country to try to address the question, “What do community health workers need in order to do their best work?” After holding listening sessions with CHWs nationwide and reviewing the domestic and international literature, her team and colleagues at NCQA developed a white paper that identifies what organizations need to do to set CHWs up for success (NCQA and Penn Medicine, 2021). Her team has also released a guide for developing sustainable career paths for CHWs (Anubui et al., 2021).
The key ingredients for success include providing training at all levels—not just a certification for CHWs but training for supervisors and program directors; providing fair compensation, supportive supervision, and manageable caseloads; and allowing CHWs to take a person-centered approach. These different domains, said Kangovi, could form the basis of national standards for CHW programs, serve as important guardrails for federal funding, and benefit CHWs.
Kangovi emphasized that CHWs are indispensable to addressing the root causes of poor health and health inequities. They can establish the relationships that need building to address social determinants; relieve workforce strain and reduce health care spending; and, perhaps most importantly, improve health for people with serious illness and even prevent it from developing.
A significant challenge is that CHWs lack a systematic way to be paid for their services, relying instead on a patchwork of grants and pilot funding. Kangovi explained that her center has been pushing for broader Medicaid coverage of CHW services and ensuring that funding is aligned with quality standards. “This will ensure that the work is high quality and that community health workers are not co-opted or over medicalized,” Kangovi explained. This policy initiative, she noted, has gained traction with the Centers for Medicare & Medicaid Services (CMS) and Congress. She noted that there are also efforts on the state and national levels to expand the CHW workforce.
In closing, Kangovi referred back to Boulware’s framing of serious illness as a story of inequity. To address that inequity, she strongly believes that
hiring and empowering those who have lived experience of that injustice is the best place to start.
Discussion Session
The discussion session, which Wang moderated, began with a conversation about wellness and the interventions that provide the greatest benefit to the health care workforce. Tucker responded that the sources of burnout are institutional and operational, including the lack of flexible work schedules, equitable compensation, ways to ensure that staff feel valued, and availability of compassionate leave time. Tucker referred to initiatives such as the Circle Up framework, staff debriefings, encouraging all staff to have grace, and being flexible as the most effective approaches because they were immediate and personal actions. Larson pointed to the importance of nursing leadership training so that nurses can have an impact on job satisfaction and quality of care provided in their units. Tucker added that role modeling by leaders is another important way for them to influence staff.
Kangovi emphasized that ensuring that people have a voice in the decisions that affect them is essential. Fowler agreed that taking steps without the whole organization’s support seemed trite and meaningless, which is why she involved frontline workers to create a compassionate leave policy for their organization. Also important, she added, is cultivating empathy and emotional intelligence among her organization’s managers and giving them the power to make exceptions for individuals to address wellness concerns.
Kangovi was asked about ways to support a diverse and inclusive community of health care workers. She replied that clinicians need to give up some degree of control and stop presuming that only people with extensive training can address health, an attitude that stems from thinking about health as a purely clinical matter. For Kangovi, moving the needle on health is less about hiring more people with thousands of hours of biomedical training and more about involving people with shared lived experience who have the empathy and flexibility to address a wide range of challenges. Tucker noted that perhaps cultural suffering should be a fifth domain of suffering that the palliative care field addresses,25 and Kangovi agreed.
Kangovi then addressed the question of what physicians, nurses, and social workers can learn from CHWs. She explained that her program pairs
___________________
25 Palliative care addresses physical, psychological, social, and spiritual aspects of care. See https://www.nationalcoalitionhpc.org/ncp (accessed March 15, 2022).
five leaders or health system executives with five CHWs who meet in a combination of small groups and one-on-one sessions. This yearlong process, has a trajectory, said Kangovi. In the first group session, all 10 people share their life story, and the differences between the health care leaders’ stories and those of the CHWs are revealing. This process allows each individual to learn about the others on a human level, which opens the door to discussing other matters on a more equal footing when the leaders shadow the CHWs and vice versa. At the end of the process, the groups work together on redesigning a specific aspect of the care system.
Wang then asked Fowler how her organization engaged in cross-training. Fowler explained that she engaged frontline workers to identify the competencies that every team member needs based on the organization’s core values. Teamwork, for example, is a core value, and according to frontline workers, it requires interpersonal skills combined with practical understanding. She noted that her organization has been on a journey of standardization to enhance its culture of safety, which served it well during the pandemic. In terms of cross-training, an example would be training nurses how to order medical equipment, something that does not require a license. Kangovi commented that health care often handicaps itself by focusing on training instead of hiring people with the proper people skills.
Perspectives on the Use of Telehealth
The second session of the webinar focused on telehealth services. Prior to the pandemic, telehealth had been used in serious illness care particularly to improve access to care in rural and underserved communities; its use was not widespread in early 2020, noted Haiden Huskamp, the Henry J. Kaiser Professor of Health Care Policy at Harvard Medical School. Once the pandemic struck, inpatient visits declined significantly, and health care systems nationwide rapidly deployed telehealth capabilities. This left clinicians and organizations that had not used it much scrambling to figure out in real time how they could best do so to maintain high-quality care.
Lessons from the Patient-Centered Outcomes Research Institute’s Investment in Telehealth Research
Steven Clauser, program director for health care delivery and disparities research at the Patient-Centered Outcomes Research Institute (PCORI), opened his remarks by noting that at the time of the webinar, telehealth
visits had plateaued, though at a level significantly higher than prior to the pandemic. In addition, telehealth growth has varied by specialty care, with endocrinology and neurology, for example, using it extensively but specialties such as orthopedics, general surgery, and ophthalmology using it to a lesser extent. According to Clauser, during the early phases of the pandemic, approximately half of all telehealth visits were related to mental health concerns.
Reimbursement and regulatory changes to eliminate barriers played a key role in enabling telehealth use to grow so quickly, said Clauser. These included changes such as lifting site of service and licensure restrictions, adding new covered services, and expanding payment parity between telehealth and in-person visits. Clauser noted that CMS recently released its final physician fee schedule for 2022, and will continue enhanced reimbursement for telehealth under public health emergency authorities.26
Referring to Boulware’s presentation, Clauser pointed out that most of the disparities in health outcomes exacerbated by the pandemic appear to be the result of access rather than care issues. “One would think that telehealth, by reducing time and geographic barriers might mitigate some of these barriers,” said Clauser. He noted, however, some indications that telehealth increased disparities in care in some cases (Rodriguez et al., 2021a,b). Clauser explained that PCORI is well positioned to provide critical information, given its $549 million support for 117 comparative clinical effective research studies in this area.27 He added that about half of the PCORI-funded studies are using telehealth to address disparities in access and health-related outcomes. They are addressing diverse vulnerable populations, with more than half of them focusing on telehealth delivery in racial and ethnic minority populations.
Clauser explained that PCORI’s broad definition of telehealth includes web portals, mobile apps, remote monitoring, and text messaging, as well as the more traditional two-way video interaction between clinicians and patients. PCORI funded 24 studies intended specifically to address the challenges of delivering care virtually during the pandemic. Nineteen of
___________________
26 See https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeeSched (accessed March 15, 2022).
27 See https://www.pcori.org/topics/telehealth and https://www.pcori.org/collection/telehealth-highlights-pcori-funded-studies-and-projects. Also see https://www.pcori.org/research-results/2020/comparing-telehealth-and-person-care-patients-chronic-conditions and https://www.pcori.org/document/changes-telehealth-policy-delivery-and-outcomes-response-covid-19-landscape-review (accessed March 15, 2022).
the studies leveraged existing infrastructure in ongoing research projects to rapidly address this public health crisis, while the other five resulted from targeted funding announcements that solicited rapid comparative effectiveness studies. Twelve addressed addiction, mental health, and social isolation; eight examined management of chronic diseases using telehealth; five looked at emerging uses of telehealth for urgent pandemic-related needs, such as infection control in nursing homes; and two focused on maternal health. (Some studies focused on more than one subject.)
Clauser discussed a study that compares the impact of two different models of palliative care—one that moves largely to care provided virtually and another that maintains in-person visits—to determine whether they provide similar outcomes to patients (Chua et al., 2019). The investigators found that clinical video visits overcame certain challenges that typically occur with in-person palliative care, including those related to time, transportation, and patient privacy.
Investigators also observed how important it was for clinicians to build rapport for difficult conversations by practicing the pace at which they conduct video visits, increasing the comfort and participation of family members, and providing technical support to the family and patients. Also important was being intentional and using what the investigators referred to as “webside manner,” which involved ensuring a proper setup for holding a virtual conversation, maintaining a conversational rhythm, responding to emotion, and concluding the visit appropriately (Chua et al., 2020). They also identified considerations that may require moving from a virtual to a phone visit, such as persistent technical difficulties, lack of the requisite technology, or patients who feel too ill to participate or feel overwhelmed by the technology required for a virtual visit.
In terms of lessons learned from the 24 studies, Clauser said the evidence regarding the effectiveness of telehealth is mixed. Despite some instances where it was clearly as effective as or more effective than the in-person approach, it failed to achieve the hypothesized benefits in a majority of the studies. Clauser pointed out that its efficacy as a care delivery mechanism depends on many factors. For example, technical issues can negatively affect the patient experience, and long-term adherence to telehealth modalities, such as remote monitoring and mobile health applications—known as mHealth—are consistently poor. These findings point to a common theme in all the studies: the importance of human support for navigating technology. The bottom line, said Clauser, is that the way in which technology is implemented is critical to its success.
Clauser pointed out that the lack of integration of the telehealth platform into electronic health records poses a barrier to clinical acceptance and thus access to specialty care. Moreover, the digital health divide, such as lack of access to broadband internet and eHealth literacy, constrains the ability of telehealth to improve access to care more broadly. Clauser noted that patient adherence to remote monitoring applications was found to be poor, and the amount of data that these generate can overload clinicians. In addition, clear protocols for managing clinical data are lacking.
Clauser shared that telehealth strategies that hold promise for reducing disparities emphasize patient-centered design and ensure that the interface is engaging and meaningful to patients who experience disparities. Clauser added that it is also important to deliver a culturally competent message that reflects the patient’s views and values. The human component can be key to the success of telehealth interventions for persons with serious illness experiencing disparities in care, and delivering care through trusted intermediaries, such as local CHWs or peers, can help to reduce disparities. In addition, patients need to be assured that the information exchanged through technology is held to the same standards of confidentiality as an interaction that might occur in the doctor’s office.
Emphasizing that PCORI’s research on telehealth is still ongoing, and themes of these early results need additional validation, Clauser concluded on a positive note: “We are hopeful that this portfolio of studies will provide evidence to answer critical questions about which telehealth strategies work best for which populations with serious illness and under what circumstances.”
Mayo Clinic’s Experience with Telehealth
Jacob Strand, associate chair for palliative care at the Mayo Clinic, opened his remarks by noting that given his position within an academic health care system, he has had a tremendous amount of resources to put into telehealth since the pandemic began. He thus cautioned that his experiences might not translate to less-resourced settings, though he was hopeful that they might at least serve as a starting point for discussion. He also explained that the palliative care program he runs has a large in-hospital consult service, an outpatient referral practice, embedded oncology clinics, primary palliative care inpatient service, and a regional hospice for approximately 200 patients under Mayo Clinic’s care in southeast Minnesota. Strand works with other leaders to coordinate and standardize palliative care interventions across Mayo Clinic’s various care settings.
Strand explained that during the pandemic, according to Mayo’s internal statistics, telehealth visits increased from less than 100 a year—mostly in a research setting—to 1,500 in 2020. In 2021, the palliative care service will have conducted 25–30 percent of its visits virtually, partly in response to patient preferences. Another factor driving this continued increase is Mayo Clinic’s strategy to grow its telehealth and virtual capacities rapidly at all of its sites and in all of its practices, with variations based on practice needs. One group is exploring integrative medicine and complementary therapies delivered by telehealth care chaplains.
From a personal perspective, Strand said he appreciates being able to blend telehealth with in-person visits. He explained that telehealth gives him the ability to see patients in their homes, have them show him where they keep their medications, for example, and see how they function at home and who is there to support them. Many of his colleagues, including physicians, nurses, advance practice providers, and pharmacists, feel differently, saying they cannot connect meaningfully with their patients via video. Strand pointed out the divergence of opinion about the best use of telehealth in some of Mayo’s sites. Areas of disagreement include whether to use telehealth only for COVID-19 patients in the ICU or whether it is appropriate for follow-up appointments after an initial outpatient consultative visit for specialty palliative care. Questions also arise about whether hospice teams should use telehealth to care for patients in skilled nursing facilities and their families.
To illustrate these differing opinions about the role of telehealth in serious illness care, Strand recalled a patient with advanced lung cancer who did not want to come to the clinic to see her oncologist or the palliative care team managing her cancer-related pain. She called when she noted some acute symptom changes, and the initial reaction of some of the outpatient palliative care team was that they could not do virtual care and wanted her to come to the ED. Others team members saw telehealth as a way to triage that visit. Conversations among team members reflected concerns about the role of telehealth in patient care and regulatory responsibilities and what conducting a virtual visit with her might mean for licensure, Strand said.
Strand explained that during the pandemic, some health care teams were using telehealth only to appropriately triage patients and provide resources to the ED, and they are continuing to operate in that manner. Others are continuing to use telehealth to interact with patients in the ICU, with one social worker working on an intervention to deliver guided imagery interventions for patients in the ICU suffering with significant dyspnea and anxiety. Some sites, said Strand, are focusing on outpatient care models,
while another site with different resources only uses it for inpatient care. He noted, too, that some providers with responsibilities for caregiving at home used telehealth so they could continue working with patients.
In Strand’s view, “this quite varied response across even a unified system, using a unified telehealth platform and medical record, is in large part a reflection of both the variation of our palliative care practices and also the types of palliative care being delivered in these sites and what each site is being asked to do by their local leadership.” Other considerations include ways to use telehealth technology to stretch limited resources based on local needs.
In closing, Strand said he views telehealth as part of a broader portfolio of technological interventions that will continue to challenge those working in palliative care. For example, greater telehealth availability may lead to more requests for his team to support patients at distant sites that lack outpatient palliative care. Such issues have led him to look carefully at his team’s practice models with a keen eye toward the sustainability of the palliative care practice overall.
Using Telehealth to Provide Palliative Care to People in Rural Areas
Pat Justis, executive director for rural health in the Washington State Department of Health, was the final presenter. Justis explained that 96.4 percent of the state of Washington is rural, with some counties that are designated as frontier areas,28 which are among the most remote and least populated areas in the nation. Justis explained that when her office began its work in 2016, the goal was to assist rural health systems and their communities to integrate palliative care into multiple settings in order to care for people with serious illness in their own communities, rather than transferring them to urban tertiary settings far from friends and family.
This project began by engaging communities to form a community-based team to collaborate on asset and gap analysis and create an action plan that included both medical and nonmedical supports for people with serious illness. This work, explained Justis, included training and coaching on clinical skills and culture change. Her team started telehealth consults and eventually progressed to direct-to-patient clinical telemedicine. Justis
___________________
28 See https://www.ruralhealthinfo.org/topics/frontier#:~:text=Frontier%20areas%20are%20the%20most,grocery%20stores%2C%20and%20other%20necessities (accessed March 15, 2022).
shared that her plan is to create rural centers of excellence in palliative care that can continue to spread on their own.
For primary palliative care, Justis’ team is focusing on building the skills and services in these rural communities. The hypothesis was that if her team used case consultation via telehealth, it could also provide secondary palliative care for more complex cases. The team could consult with a tertiary expert team for more complex cases.
Justis shared a key lesson learned from her team’s experience, notably the importance of having community-based team members structure and design the care that needs to be provided given that they are experts in the needs of their own communities. She explained that to be successful, telehealth consulting experts must affirm the skills they see, offer empathy for how difficult cases can be, and give the rural teams room to engage in dialog with the expert panel. Telehealth case consults began operating at two levels: improving clinical care for a patient and engaging in generalizable education. Justis noted that rural health teams were already caring for complex patients and relished the assistance from telehealth consults. “Their knowledge and concern for these patients is remarkable and never fails to touch us all during these sessions,” observed Justis.
Justis referenced Clauser’s earlier remarks about the importance of assisting people with technology, particularly in areas with poor or limited broadband access. Justis explained that her program supported patients with hot spot tablets and team members made home visits to teach relevant skills. The program switched to having a nurse or other clinician be in the patient’s home while the rest of the team is virtual, which seemed to work better than expecting a patient to do this independently, said Justis. She noted that when the direct clinical telemedicine pilots began, her teams’ confidence had grown such that the rural teams decided to use telemedicine for their own patients rather than relying on a distant urban tertiary team.
Other lessons learned included the importance of having both a nurse clinical coordinator and a technical coordinator. The clinical coordinator, said Justis, works with the various cohort teams to prepare them to present a case, which helps the teams have confidence and refine how they are going to deliver the case. Training, she added, has focused heavily on communication skills and less so on symptom management, and the telehealth consultant provided the rural teams with the opportunity to observe interdisciplinary teamwork in action. “We are fortunate to have a medical director for the project who is probably the most egalitarian, team-based individual I have met in my career, and he models that beautifully, along
with the other team members,” said Justis. She noted that her team works closely with the Washington State Hospice and Palliative Care Organization, and this collaboration has prompted that organization to begin exploring how to deliver services in other areas using telemedicine.
Justis pointed out that the pandemic helped the 13 pilot sites jump faster from planning to testing and implementation of telemedicine palliative care visits. Rural health organizations are proceeding with expanded telemedicine as a prime mode for palliative care, and her office will continue providing the expert panel to guide and train rural health teams.
On a final note, Justis explained that the public health emergency waivers for telehealth were important for rural areas because they enabled rural health clinics and federally qualified health centers to serve as both originating and distant sites for care. Also helpful for providing telehealth in rural communities was CMS’ relaxing Medicare location requirements, establishing payment parity for Medicare telemedicine visits, and allowing for voice-only visits, which is particularly important for areas with poor or no broadband access.
Discussion Session
Session moderator Huskamp opened the discussion session by asking the panelists to comment on the use of voice-only visits to care for people with serious illness and reimbursement for such visits going forward. Justis replied that it is critical to base the decision on patient preference. Strand and Clauser added that voice-only consults could be useful for those who cannot use video technology. In addition, said Strand, it can be challenging technologically to deliver care via video with a team-based approach, while conference calls are simple to conduct.
Tucker, who spoke in the first session, noted a considerable amount of concern about overuse of telehealth, particularly for opioid management. “I think we have a technology that is going to add to the menu and have many, many good aspects, but it is not a savior for access. It could potentially even worsen disparities, because some folks do not want to use technology,” he said. He worries that people who lack broadband access and only have prepaid phones will begin to feel marginalized because they cannot take advantage of these opportunities.
Regarding reimbursement, Strand said it is a critical issue if telehealth is to be sustainable. Clauser noted that prior to the pandemic, neither CMS nor private insurance paid for voice-only visits, making this unfamiliar ter-
ritory for insurance companies, health plans, clinical teams, and patients. He added that the research on this topic is emergent, and that even though CMS reluctantly agreed to continue funding voice-only visits for another year, he doubted that private insurance would allow that option over the long run.
Huskamp noted that some have argued that the costs of delivering services via telehealth are lower than for in-person care and therefore telehealth should be reimbursed at a lower rate. Justis said that her cohort members have told her that it takes just as much time and coordination to prepare for virtual visits, so telehealth is still time intensive. Clauser added that research is showing that it takes a great deal of work to prepare individuals with low health literacy for telehealth visits. His worry is that making such a comparison might lead to missing an opportunity to provide the human support needed to help them use the technology.
When asked about tools, websites, or programs that can help older persons and others who are technology challenged, similar to the services that Senior Planet and the AARP hotline provide, Justis said Northwest Telehealth has developed a tool kit for preparing to engage in telehealth. Though it is not specific for older adults, it is patient centered. Clauser said that the national children’s hospitals have created websites to help facilitate telehealth for parents who were nervous about exposing their children to COVID-19 in clinical settings.
Strand addressed a question about barriers to engaging in telehealth from the health care provider perspective, by noting that while most of the clinicians on his team have picked up the technology quickly, some colleagues miss the hierarchy that exists in being the doctor who comes into the office. Similarly, clinicians have reported missing the ability to engage with a colleague down the hall or bring a social worker or chaplain into a visit. As a result, his team is working to build out some of its care models to allow clinicians to bring in colleagues when needed to augment a visit. Justis pointed to the importance of having someone supporting the technology who can do so with a sense of warmth and without making people feel on the spot or ashamed. Clauser added that clinicians are right to be cautious given that specialty societies have not yet promulgated standards and guidance on what works and what does not, despite a developing evidence base. Missing, too, are the quality measures and approaches for measuring accountability for good telehealth interactions that exist for in-person clinical care.
Huskamp asked about a role for a hybrid virtual/in-person model. Justis replied that the Providence Health System in the northeast corner of the
state is having success with a blended model in which a board-certified palliative care physician and an experienced person with a Ph.D. in social work and expertise in behavioral health and palliative care join a teleconference with a local team that is physically with the patient. Strand added that as a palliative care clinician, the more he could collaborate with the clinicians who are primarily managing a patient, the more care he could help deliver. Noting that such partnerships have been meaningful experiences for him, he added that he hopes that research will identify measures for the quality of such visits that will help improve the quality of outcomes.
Clauser noted that all the protocols PCORI is funding involve hybrid models. He added that the performance of virtual care starts diminishing over time, suggesting a need for occasional in-person visits so the clinician and patient can reconnect. This area requires further study to determine the “dose effect” that can lead to a good hybrid model, particularly for frontier communities.
One issue Strand sees is the need for guardrails to protect clinicians from being accessible all the time. Huskamp asked Strand if the demand for palliative care consults have increased as clinicians have seen the value of palliative care during the pandemic and, if so, if that is affecting how his organization uses the palliative care team. Strand replied that demand has increased and his organization is now looking at the investments needed to fulfill it. Insufficient clinicians are trained in palliative care, and it would require large investments to develop that workforce. His team is using artificial intelligence and machine learning to analyze patient-reported outcome data to figure out which patients could benefit most from a palliative care specialist versus a mental health counselor, CHW, physiatrist, or occupational therapist.
Justis said that helping the rural health care workforce develop palliative care skills is critical to meet the needs of rural communities. However, that workforce needs to recognize its limits in terms of determining which patients’ needs they can handle and whom they need to refer to palliative care specialists.
As a final question, Huskamp asked the panelists to identify one or two barriers to delivering serious illness care via telehealth. For Justis, broadband expansion in areas with low population density is critical to reducing disparities for those communities. Strand said that differences in state licensure requirements represent barriers to telehealth. Clauser added that reimbursement can be a barrier, particularly when it comes to the extra human technical support that patients with low literacy need to engage in telehealth.
Closing Remarks
Wang concluded the webinar by observing that the speakers highlighted the need to prioritize the health care workforce and patient safety, the imperative to integrate equity into core health care structures, and the need to identify models of care and policies that will lead to optimal care delivery. Equipped with these and other lessons, the nation could better prepare for future pandemics. Wang closed the webinar on a hopeful note, pointing out that although the pandemic has brought many challenges for people with serious illness, it “can be a force that helps transform our health system for the better.”
WEBINAR THREE
Bowman opened the final webinar in the series by explaining that the first session would focus on public health communication and research translation. The second session would attempt to synthesize the many key messages that were raised throughout the webinar series, with the hope that it would serve as a call to action for strengthening the care of people with serious illness.
Public Health Communication and Research Translation
The third and final webinar took on two main topics. The first session focused the challenge of public health communications during the pandemic in general and for specific populations, such as pediatric patients and racial and ethnic minority groups. In the second session, the panelists looked to synthesize the key themes and lessons learned into a call to action, for both policy makers and health care providers, for improving care for people of all ages and all stages of serious illness.
Keynote Address
Ashish Jha, dean of the Brown University School of Public Health,29 opened the webinar with a keynote address focused on the importance of public communication in a health crisis, the pitfalls of public communica-
___________________
29 Dr. Jha has since been appointed White House coronavirus response coordinator; this temporary special assignment began April 5, 2022.
tion, and some of the challenges scientists, public health officials, and public health academics have in communicating effectively with the public. He also offered some ideas about how the scientific and public health communities might do this better in the future. He began his remarks with the most basic question: Why communicate with the public at all? “Certainly, getting the science and evidence and policy right is central, but communicating with the public is always important, and particularly so in a health crisis,” emphasized Jha.
Jha explained that in a health crisis, ordinary people must do extraordinary things. “These are extraordinary moments where we have asked people to fundamentally alter the way they live their lives, the way they see their loved ones, the way they engage in their work, and the way they engage with school,” said Jha. “This is hard stuff to ask people to do, and in general, under most circumstances, people will not say yes unless there is a compelling reason.” Two years ago, he added, asking people to wear masks in indoor spaces would have been odd, but today it is routine. He also noted that more Americans have learned about testing, quarantining, and isolation in the last 2 years than they ever had before.
While getting mayors, governors, and presidents to make effective policies is a key step, implementation of and adherence to such policies requires explaining to the public what the underlying issues are and why they need to change their habits and behaviors. To do so requires an extraordinary effort at public communication and training on the part of the expert communities. “I would argue that most of us in public health, most of us in science, and most physicians have not been trained on how to do that effectively,” Jha noted.
Jha pointed out that 2 years ago, if asked what the expert community should do during a health crisis, he would have responded that the main job of public health in terms of scientific communication would be to get the science right, get the data right, figure out the evidence, synthesize the evidence, and then explain it to the people in a way that makes sense. His belief, in short, was that the facts, evidence, science, and data would alter the public’s behavior.
Acknowledging how naïve that sounds today, Jha noted that there is still some truth to this belief: facts and evidence do matter to people. However, a major lesson from the pandemic has been that for people to change what they do, it is not enough to give them facts. “It is also about understanding and addressing things that they value and find meaningful, and that requires an understanding of a variety of things that we in public
health and in science have largely not been trained in,” said Jha. Going on television or participating in town halls and regurgitating evidence is not going to alter public behavior. “We have to understand the fears that people have, the anxiety people feel, and we have to understand what is going to motivate people to do things that are going to be in their own best interests and their own best health,” he added.
Fortunately, behavioral scientists have identified effective approaches to encourage people to change their behavior. Unfortunately, most people in public health and science communication have not learned those skills, which led to problems during the pandemic. Jha pointed out that widespread misinformation and disinformation is not uncommon during a pandemic. “Anti-vaxxers,” he noted, have been around as long as vaccinations have, going back to the days of smallpox when groups pushed back against inoculation. Jha explained that the 1918 influenza epidemic saw the rise of an anti-mask movement, making exactly the same nonsensical arguments then that today’s anti-maskers raise about how masks cause their own infections and pose a health danger by retaining carbon dioxide.
Jha further explained that misinformation thrives in situations of high levels of uncertainty and an information vacuum. Those who peddle misinformation have become very adept at identifying those moments and offering up information and ideas that feel right, even if they are not. “That, by the way, is a truism throughout all of history,” said Jha. “That is not a phenomenon of the COVID-19 pandemic or the twenty-first century.” Pointing to the echo chambers in which everyone lives as an example of a twenty-first-century phenomenon, Jha explained the way information is disseminated creates self-perpetuating, self-enforcing information echo chambers where one bad idea can take hold, get amplified by multiple actors, and then become “gospel truth,” explained Jha.
There is also disinformation (information promulgated by bad actors who are purposefully creating it to create confusion), noted Jha. Domestic as well as foreign groups have essentially “weaponized misinformation,” said Jha, tainting the information ecosystem for political motives or even profit. Jha noted that the only way to address these sources of disinformation is to tackle them on the platforms they use. “This is a responsibility of Facebook and Twitter and Google to deplatform these folks, because there is no engaging them,” he said. “This is asymmetric warfare that requires a very specific response,” Jha emphasized.
It is impossible to counter all the disinformation, but the scientific and public health expert community could take certain steps to be more
effective in the information ecosystem, explained Jha. This requires understanding how scientists, physicians, and public health officials struggle with science communication. Jha shared that when he was trained as a scientist to write or talk about his work, for example, he learned to discuss the limitations of his research, uncertainty in the findings, and exceptions that might make his findings null or not fully applicable. “This is how science works, and it is a good thing for the scientific process,” said Jha, “but it does not work well in public communication.”
Jha pointed out that the expert community has not done an adequate job of communicating to the U.S. public that science is a process. When experts say, “follow the science,” they do not mean follow a finding that will be true forever but rather follow the process and see where that leads. The scientific community needs to make the public understand that they know certain things at a given moment and learn more over time but without overemphasizing all the uncertainties and unknowns. “My general approach on this has been to recommend that we talk about what we do know and then provide judgment about the areas where there is more uncertainty,” said Jha. In other words, “Explain the uncertainty, do not hide it, but at the same time provide judgment.”
As an example, he noted that when the data about mRNA vaccines came out, a big question on people’s minds was whether they would slow or reduce transmission. Most experts said they did not know, because the studies had not yielded definitive results. However, most Americans did not hear that as “we do not know that vaccines reduce transmission” but rather that “the vaccines do not slow or reduce transmission”; for months, this was the broad consensus in the United States, even though it was not true. A more effective answer, said Jha, would have been that while it is not certain that vaccines reduce transmission, it is likely because that is what most vaccines do. Preventing infections most likely reduces transmissions as well. “I think there is a way to communicate that gives people a judgment about what is likely to be the case without overstating what you do and do not know,” he said. It is through that process that he believes the expert community can begin to train people to understand the scientific process. “I think that is actually absolutely critical and is something we have not done enough of,” added Jha.
One part of public communication is talking about uncertainty in ways that are more helpful and less nihilistic and explaining the process of scientific learning and discovery. Another important piece, which many people in the science world find uncomfortable, is to connect with the public based
on personal experience. Jha shared that one of the more effective tools he uses for important questions is to start his answer with his own personal decision and then explains why he made it based on the evidence. Taking this approach, said Jha, helps people feel more in touch with the data and enables them to have more confidence in it.
A critical aspect of communicating science to the public in conditions of uncertainty, said Jha, is explaining what evidence is needed to address that uncertainty. For example, people ask if they will need another booster in 6 or 12 months, and the short answer is “we do not know.” However, the better answer would be “we do not know because we have not had enough experience yet, but there are studies going on that are tracking people who have received boosters to look for waning immunity, and those studies will provide answers in 3 months, 6 months, and 12 months.” That second answer provides a sense of when that uncertainty will lift, accurate information, and a framework for understanding what is happening. “It also makes them far less susceptible to misinformation than when someone shows up and says, ‘I know the answer today,’” said Jha.
In closing, Jha reiterated that effective public communication of science information is central to combating both misinformation and disinformation, both of which thrive in information vacuums. “When we get outside of the scientific community, when we begin to engage with the public, it is absolutely critical to help Americans understand the scientific process, communicate both uncertainty and certainty, communicate judgment, personalize it whenever that feels appropriate so people know that this is not generic advice but is advice you would take yourself.” Jha explained that the scientific and public health community can “really build the trust and confidence that people need to fundamentally change their behaviors, because that is what we are asking people to do. We are asking people to do things they would never do before under normal circumstances, and that fundamentally requires trust,” concluded Jha.
Discussion Session
Pamela Hinds, executive director in the department of nursing science and research integrity officer at the Children’s National Hospital and professor of pediatrics in the School of Medicine and Health Sciences at George Washington University, asked Jha to comment on a situation in which he regrets a personal decision related to teaching the public about science. Jha replied that he has given advice and had it turn out to be wrong when the
evidence changed. Referring to his earlier example about whether a booster shot would be necessary, he explained that 6 months ago, his response based on the evidence would have been that it was not. When the evidence changed, however, he had to acknowledge that it and the recommendation changed. He said that it is important to remind people that this is how they want their physicians to practice medicine in response to new evidence.
Jha shared that sometimes, however, he honestly gets things wrong. “There is a barrage of information, and I have found that people generally do not penalize you for getting things wrong,” said Jha. “They penalize you when you are not willing to own up to it, whether it is on social media, Twitter, or television.” The key is to be open and acknowledge the error, just as a researcher would do if they found an error in a submitted paper. This builds long-term credibility.
Hinds then asked Jha if his approach to science communication changes when dealing with those who are involved with misinformation or disinformation. Jha replied that the first step is to understand what motivates people to create and spread misinformation or disinformation, and those motives differ. Disinformation is well planned and organized, often by foreign actors, and that requires a very specific set of interventions that go beyond what he is able to do, which is why he talks about the things that Facebook, Twitter, YouTube, and other information outlets have to manage.
Regarding misinformation, two groups are involved in Jha’s view. One group has an ulterior motive, such as something to sell. Someone in that group might spread misinformation about vaccines because they have a tonic they are peddling as a cure for COVID-19. The second, larger group includes people who believe misinformation based on what they hear, and the key to dealing with those individuals is to understand why certain types of information are accepted without question by certain groups of people.
In terms of the timing for engaging in a communication intervention, Jha used the exact situation at the time of this webinar, when the Omicron variant was first identified in South Africa, creating a great deal of uncertainty and anxiety with minimal information available. “If all the scientists said, look, we do not know anything and we are not going to talk about it until we know more—call us back in 2 weeks—that would not work for two reasons,” said Jha. “People feel anxious now, and if you do not fill the information gap, there will be plenty of people with far less knowledge who will be happy to step in and spread misinformation.” The expert community needs to be willing to speak even when it does not know the answer.
The best way to counter misinformation, according to Jha, is with good information, which requires everyone in the science, medical, and public health communities to take a role in spreading it. This does not necessarily mean going on television; town halls and local meetings can also provide good avenues. “What I would say to everybody who is listening is ask yourself, in a crisis like this where information is at the heart of the crisis we are in, how do you play a role in spreading good information? How do you play a role in bolstering good information? That is a critical job that we all have,” concluded Jha.
Lived Experience
Daniela Lamas, an instructor in medicine at Harvard Medical School and associate faculty at Ariadne Labs, provided an overview of what it was like in her hospital during the early days of the pandemic. Arriving at work in April 2020, Lamas noticed that her unit had been transformed. The doors to each patient room were closed, with a ventilator monitor sitting outside each room. Intravenous poles crowded the hallway, and nobody wanted to enter those rooms. Some doors had a small collage on them, a get-to-know-me poster with the patient’s name and a photograph of happier times and facts that now feel entirely incongruent. “It is something, but a poor approximation of how it used to be with families at the bedside eager to tell you a story about the person you are taking care of,” said Lamas.
The rooms were empty save for a patient, whose face she might have never seen, since they would be lying on their stomach or turned to the side. Nurses in the hallway tried to tell her something, but she had a hard time hearing through their masks. One of her COVID-19 patients had taken a turn for the worse, and staff decided to allow his wife to visit. Lamas explained that it had been weeks since the woman had seen him. Lamas was worried because she had offered reassuring words every day and knew that a visit would destroy that false picture of stability.
The patient’s wife told Lamas that she had been reading and wondered if her husband could get convalescent plasma. Lamas took out her patient list, wrote “palliative care” next to his name, and told his wife that the palliative care team would be around later to help her navigate what was to come. Immediately afterward, she received a page from the ED—it was an overdose, not related to COVID-19. That patient was able to go to the regular ICU, but it was a reminder that other health crises continued during the pandemic. Lamas observed that in the early days of the pandemic,
everything moved so quickly that there was barely any time during rounds for anything more than practical questions, such as when to intubate, when to use high-flow oxygen despite the risks to the patient, and whether it was irresponsible or humane to try to sneak in an extra family member overnight.
Today, said Lamas, different questions have begun to emerge, such as what went well and what did not. “As we all move toward some sort of new normal and try and grasp at post-traumatic growth to make meaning of the past 18 months, what lessons can we take for how to care for seriously ill patients?” she asked.
Before the pandemic, the ICU was a place where families observed procedures and sometimes even resuscitation attempts, in large part because staff had come to recognize that families were not just visitors but essential members of the care team. But once the pandemic hit, family members were gone, Lamas explained.
Though the threat from the virus has changed, family members are not coming back in large numbers, and Lamas wonders what lessons can be derived from their absence. Though the studies on this are starting to appear, Lamas said that without families, the hospital is quiet, and she and the rest of the ICU staff struggle to know their patients as more than a list of diagnoses. She also believes that staff is missing subtle and potentially meaningful clinical changes, such as signs of a stroke in a patient that the ICU staff would have caught earlier if a family member had been at the bedside. For families, she wonders if she can forge the trust in a phone call that once was built over hours and days at the bedside.
Lamas shared that in her view, family members have not been brought back quickly enough, particularly for those in the ICU. “I think there is a real inflection point here in terms of our acknowledging that family members are not just visitors for the seriously ill in the hospital but they are an essential aspect of the care that we deliver,” said Lamas, who hopes that this will not be a forgotten lesson. A similar lesson is the importance of preparing an advance directive and a medical power of attorney or health care proxy, regardless of how young or healthy an individual is. She noted that she had many conversations with health care proxies she had never met in person and yet who had to trust her even when she was not sure she could trust herself. Echoing earlier speakers, such as Fineberg and Jha, Lamas noted that “navigating uncertainty and gaining trust despite uncertainty became key in this pandemic… There was so much fear, fear of the virus
but also fear on the part of families of interventions being withheld, fear of the scarcity of equipment, and fear that we were giving inaccurate information. And as for us, the physicians and nurses, the fear was that we were not giving the best possible care.”
Lamas noted that, in the early days of the pandemic, those fears led her to reflect on what she did not yet know about delivering the best care during a pandemic and on what she and her team did know about the components of high-quality critical care. “We know about waking patients up every day, minimizing sedation, meticulously monitoring labs and ventilator settings, but in the early months of the pandemic, we let fear take hold and set our protocols aside,” she said. She accepts that this was understandable but acknowledged it as an error. “When faced with serious illness and with fear and misinformation, we must make sure that no matter what else is going on, we do not lose sight of life-saving fundamentals that we do know,” she added.
Lamas observed that for those who survived the virus, the pandemic taught them a final lesson: surviving serious illness is not the same as recovering. In critical care, the focus has been on mortality, with research paying less attention to quality of life. That focus has produced new diagnoses, such as post-intensive care syndrome, and an understanding about a growing population of people with long-term dependence on a ventilator or other life support technologies. Public understanding is growing that mortality is not the only outcome that matters, and she and her colleagues in ICUs must shift their conversations to account for that change. “The broader system must ensure that there are ongoing conversations through the entire trajectory of care for those who do press forward with aggressive interventions,” said Lamas.
As a concluding thought, Lamas said that the pandemic tested the system’s ability to care for seriously ill patients in a way that no other public health care in her lifetime has. “It showed us devastating truths about the fault lines in our country’s belief in science and medicine, showed us that fact can be politicized,” said Lamas. “But that was not its only impact,” she continued, “for it also broke down the divide between our patients and ourselves, forcing us to realize that anyone at any time could become seriously ill, and forcing us to see the extent to which we are all truly interconnected.” Lamas concluded that her hope is that the health care community will take all the critical lessons learned during the pandemic and use them to improve care.
The Impact of COVID-19 on the Pediatric Population
Roberta Lynn DeBiasi, chief of the division of pediatric diseases at Children’s National Hospital and professor of pediatrics and microbiology, immunology, and tropical medicine at George Washington University School of Medicine and Health Sciences, began her remarks by describing how the initial reports during the early stages of the pandemic suggested that COVID-19 was not affecting children. She noted that the world of pediatric ICU infectious disease specialists is close-knit, and none of her colleagues around the country were seeing cases of infection among children.
That all changed, however, when the pandemic hit the U.S. East Coast. DeBiaisi and her colleagues began seeing a significant number of infections and hospitalizations of critically ill children, along with the emergence of an inflammatory disorder affecting children. Almost immediately, the American Academy of Pediatrics and the Children’s Hospital Association, which has over 40 hospitals that care for children exclusively, began compiling state-level data. At the time of the webinar, DeBiaisi explained, children accounted for more than 25 percent of all COVID-19 cases, but the vaccine was not yet approved for all age groups.
DeBiasi further explained that she and her colleagues at Children’s National Hospital had seen over 4,000 symptomatic children, with over 800 who required hospitalization. One-third of those hospitalized were critically ill and spent time in the pediatric or neonatal ICU. Just as staff had figured out how to care for these children, a new disease emerged that is unique to children—multisystem inflammatory syndrome (MIS-C)—that seems to lag circulation of COVID-19 in a community by 4–6 weeks. DeBiasi pointed out that two-thirds of the 200 children with this condition who have been treated at her institution have required major life support (DeBiasi et al., 2020).
DeBiasi described how she realized early on that she and her colleagues had to educate the public about their experience with pediatric patients, to encourage parents to look for the signs of severe illness and prepare hospitals for the potential influx of pediatric patients with unique needs. DeBiasi explained that as the pandemic hit parts of the country in waves, the pediatric community was able to widely share its knowledge internally. She noted that researchers at her institution, for example, were the first to report and confirm that the racial, ethnic, and socioeconomic disparities seen in adults also occur in children (Goyal et al., 2020).
When the first reports of MIS-C came out of the United Kingdom, DeBiasi and her colleagues were on the phone and in conference calls to
decide if this was Kawasaki disease or a new disease.30 Within 24 hours of these calls, the whole East Coast started seeing nearly identical cases. “We are so thankful to them for raising this awareness because we were able to recognize these cases and start optimizing the care of the children, which has dramatically reduced the number of deaths from this really devastating disease,” she said. She and her colleagues recently published a compendium not only looking at the epidemiologic and socioeconomic factors in these children but also defining different ways that they can present (DeBiasi, 2021; DeBiasi et al., 2021). Given that all cases do not look the same, DeBiasi explained that this publication improved how the pediatric community cares for these children.
DeBiasi observed that at the time of the webinar, the United States had seen over 5,500 cases of MIS-C and 48 deaths, with Black/African American and Hispanic/Latinx children accounting for 46 and 35 percent of cases, respectively. She and her colleagues are following her institution’s initial cohort of MIS-C patients to identify any long-term effects. In the meantime, CDC has created informational materials that pediatricians and family practitioners can use to alert parents about the early signs of MIS-C.
Misinformation about vaccines is significantly amplified in the context of caring for children, DeBiaisi pointed out. On the one hand, she explained, pediatricians and public health officials are telling parents that children have only a 4 percent chance of being hospitalized and an even lower chance of death, while on the other hand, parents are hearing about myocarditis arising from one of the vaccines. In fact, she said, in her institution’s 5- to 11-year-old age group, almost 10,000 have been hospitalized and 100 have died, so children are at risk. “Even though 4 percent is a low number, when we look at the total amount of infections that occur in this age group, it is a realistic risk that there could be a significant number of hospitalizations or deaths if these children are not vaccinated,” she said. DeBiasi also pointed out that a study of over 2,000 children has shown that
___________________
30 According to the CDC, “Kawasaki disease (KD), also known as Kawasaki syndrome, is an acute febrile illness of unknown etiology that primarily affects children younger than 5 years of age. The disease was first described in Japan by Tomisaku Kawasaki in 1967, and the first cases outside of Japan were reported in Hawaii in 1976. Clinical signs include fever, rash, swelling of the hands and feet, irritation and redness of the whites of the eyes, swollen lymph glands in the neck, and irritation and inflammation of the mouth, lips, and throat” (CDC, 2020). See https://www.cdc.gov/kawasaki/about.html#:~:text=Kawasaki%20disease%20(KD)%2C%20also,reported%20in%20Hawaii%20in%201976 (accessed March 8, 2022).
vaccines have a 91 percent31 efficacy rate at preventing symptomatic disease even though the children received one-third of the adult dose. Despite these results, DeBiasi observed that at the time of the webinar, vaccination rates among the group of children (5 to 11 year olds) that was recently approved for the vaccine were low.32
DeBiasi noted that while there have been cases of long COVID among children, it is not clear whether it has the same impact as it does on adults. DeBiasi and her colleagues, together with researchers at the National Institute of Allergy and Infectious Disease, have embarked on a 3-year study to track the prevalence of long COVID in children.33 The research team will conduct extensive patient evaluations, including pulmonary, cardiac, neurodevelopmental, quality-of-life, and mental health assessments; develop a biorepository; and examine a variety of scientific research questions about host genetics, T cell responses, and antibody kinetics.
DeBiasi pointed out that COVID’s impact on children and families extends beyond its direct effects. The secondary challenges include housing instability, which will grow worse as eviction bans expire; increased child care demands as parents return to in-person work; food insecurity; behavioral health issues resulting from the dramatic increases in pediatric depression, anxiety, and eating disorders; and the increase in obesity and type 2 diabetes as children become more sedentary. DeBiasi also noted that loss of learning is a particular problem among Black and Brown students who have been affected disproportionately by the move to virtual instruction during the pandemic.
National Institutes of Health’s Efforts to Reduce COVID-19 Health Disparities and Distrust
Monica Webb Hooper, deputy director of the National Institutes of Health (NIH) National Institute of Minority Health and Health Dispari-
___________________
31 See https://www.mayoclinic.org/diseases-conditions/coronavirus/in-depth/covid-19-vaccines-for-kids/art-20513332#:~:text=Among%20663%20children%20given%20the,children%20in%20this%20age%20range (accessed March 8, 2022).
32 As of December 15, 2021, the CDC reported that 5.6 million U.S. children ages 5–11 had received at least one dose of COVID-19 vaccine, representing 20 percent of 5–11 year olds. See https://www.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/children-and-covid-19-vaccination-trends (accessed March 8, 2022).
33 See https://childrensnational.org/news-and-events/childrens-newsroom/2021/cnh-and-niaid-launch-large-study-on-long-term-impacts-of-covid-19-and-mis-c-on-kids (accessed March 8, 2022).
ties (NIMHD), opened her remarks by explaining that health disparities are a particular type of health difference that is closely linked with social, economic, and/or environmental disadvantage. They adversely affect groups of people who have systematically experienced greater obstacles to health based on their racial or ethnic group; religion; socioeconomic status; gender; age; mental health; cognitive, sensory, or physical disability; sexual orientation or gender identity; geographic location; or other characteristics historically linked to discrimination or exclusion. The distinguishing factor of health disparities compared to other forms of differences, such as population differences, is that disadvantage is the causative agent. “Importantly, in contrast to general population differences, health disparities are differences that should not exist and that are modifiable, which means that we have the opportunity for change,” said Webb Hooper.
Referring to Boulware’s presentation in the first webinar, Webb Hooper explained that most health conditions have considerable racial and ethnic disparities, including shorter overall life expectancy; higher rates of cardiovascular disease, cancer, diabetes, infant mortality, stroke, cognitive impairment, asthma, sexually transmitted infections, and dental diseases; and differences in the prevalence and outcomes of mental illness. Webb Hooper noted that she and two of her colleagues published an editorial on racial and ethnic COVID-19 disparities that made the point that the pandemic has served to shine a light on health disparities, creating an opportunity to address the root causes of underlying inequity by using culturally appropriate and community-competent strategies (Webb Hooper et al., 2020). These strategies must consider the nuances of populations, communities, families, and individual differences, all of which have a vital role in reducing health disparities by promoting health equity and improving population health.
Webb Hooper observed that early in the pandemic, scientists, physicians, and health officials often noted medical comorbidities as the cause of disparities, and racial and ethnic minority populations have a disproportionate burden of underlying comorbidities. Webb Hooper emphasized, “Race is a sociocultural construct, not a biological or genetic one, and race is important to study because it shapes the lived experiences of all groups. It is important, then, that we consider the full context, which includes systemic factors, such as historical and ongoing discrimination, chronic stress and its effects on immunologic functioning and health, and others.”
A key point, she continued, is that disparities in COVID-19 are not occurring because racial and ethnic minority groups are inherently more susceptible to the virus. Rather, they result from social inequities that have
given rise to higher rates of preexisting conditions, such as heart disease, diabetes, and HIV. This points to structural issues rather than inherent biological or genetic underpinnings. Webb Hooper identified trust as an underappreciated social determinant of health. “COVID highlighted distrust in addition to the social justice issues happening in the country,” said Webb Hooper.
Webb Hooper then focused on the work of the Community Engagement Alliance (CEAL) Against COVID-19 Disparities.34 This NIH-wide initiative is focused on outreach and engagement efforts to address distrust, particularly among racial and ethnic minority groups disproportionately impacted by the pandemic. CEAL’s immediate priority was to address disparities and diversity in clinical research trials, particularly the COVID-19 trials that launched in summer 2020. A lack of diversity is a perennial issue; as an example, Webb Hooper noted a kidney cancer therapeutic trial in which only 5 of the 821 participants identified as Black or African American (Motzer et al., 2015).
Webb Hooper explained that one issue she and her colleagues have focused on since the beginning of the pandemic is how to increase trust in biomedical science and health care. “We do know that expertise from multisector stakeholders, including those from affected communities, is important,” she said. “We need individuals who can deliver the right messages, and community groups and other experts are among the right messengers to help build trust.” Those stakeholders, she added, also have important insights about the members of their communities. Webb Hooper described a number of approaches to effectively increase trust and participation in clinical trials, such as diversifying the care team, setting a priori targets for recruitment, developing a multifaceted recruitment strategy, engaging the community in a bidirectional manner, and establishing trust as the foundation. Additional approaches include addressing the social and structural determinants of health, acknowledging the long-standing, and earned, distrust of medical institutions and biomedical research, and approaching the community with cultural humility. Above all, Webb Hooper said, simply asking people to join a study is an effective strategy.
As CEAL was beginning its work, NIH leadership worked closely with Moderna on its COVID-19 vaccine trial to focus on increasing enrollees’
___________________
34 See https://covid19community.nih.gov (accessed March 15, 2022).
diversity.35 NIH leadership and subject matter experts provided guidance about the aforementioned strategies. Moderna’s team made some adjustments, explained Webb Hooper, and racial and ethnic minority inclusion improved over time. At the trial’s conclusion, the proportion of racial and ethnic minority individuals was significantly higher than most industry-led clinical trials, with Black and African American and Hispanic/Latinx individuals accounting for 10 and 20 percent of participants, respectively. Webb Hooper noted that Moderna acknowledged the role of NIH and CEAL in increasing the diversity of the trial’s participants.
The CEAL initiative is ongoing, with the alliance engaging in activities across its 23 locations nationwide to establish partnerships with communities, address misinformation, increase trust in science, and accelerate uptake of beneficial interventions, including vaccines. All of these efforts focus on tackling the disproportionate burden of COVID-19 on racial and ethnic minority populations. Webb Hooper noted that CEAL’s website contains a repository of valuable information to help combat what she referred to as the “COVID-19 infodemic.” The materials are available in multiple formats and in Spanish, and may be customized for local or community contexts.
Webb Hooper emphasized that researchers need to recognize that racial and ethnic minority groups, in general, are just as willing to participate in clinical trials, which several well-conducted trials demonstrate. In fact, she said, NIMHD could not exist if that was not the case. “It is important to dismiss the notion that these groups are just not interested in participating or are just hard to reach,” she said, and to identify the best approaches for reaching marginalized communities. “Maybe we just have not done enough, in terms of the health care system and researchers, to ease the minds of populations around research and to address the institutional distrust that exists,” she concluded.
Discussion Session
To open the discussion session, Hinds asked Webb Hooper how she can talk about a tragic experience, such as the pandemic, and still think about it in terms of opportunities. Webb Hooper replied that because the pandemic
___________________
35 See https://www.nhlbi.nih.gov/news/2021/researchers-take-cues-past-ensure-diversity-covid-19-clinical-trials (accessed March 15, 2022). Also see https://www.kff.org/racial-equity-and-health-policy/issue-brief/racial-diversity-within-covid-19-vaccine-clinical-trials-key-questions-and-answers (accessed March 15, 2022).
has laid bare the inequities in the health care system and the disconnect between public health, science, and medicine, she and her colleagues at NIMHD are seeing an unprecedented level of national attention to and discourse about disparities. This attention creates an opportunity to inform, educate, and think about ways to address these inequities.
Hinds then asked DeBiasi how she provides information about COVID-19’s effects on children without creating panic. DeBiasi explained that in the pandemic’s initial phases, the public was aware of the severe impact of COVID-19 on adults, and as soon as people heard it was not a serious concern for children, an out-of-sight, out-of-mind attitude developed and parents stopped thinking about it as a threat to their children. When children began becoming seriously ill, however, the media focused on the most extreme cases. Parents were confused by conflicting messages. DeBiasi pointed out that her approach was to provide accurate, up-to-date information and then empower parents, telling them they know their children better than anyone else does. If their child looks seriously ill to them, get them to care, but do not rush to the ED every time their child looks sick. If their child looks fine but has a runny nose and a cough, they should not worry because this is typical of the overwhelming majority of children with COVID-19. Referring to an earlier comment by Jha, DeBiasi noted that she always talks about this information in the context of her own experience as a parent. In fact, when she gives weekly situation updates, her last slide is always about something that happened in her own family. “It really does help people to see that we are navigating the same information in our own families and with our own kids,” said DeBiasi.
Hinds asked the panelists about the strategies they use to cultivate trust. DeBiasi said that one should not assume that someone from a different background or belief system has grounds to trust someone just because they are a physician. She recounted how serving on the DC Vaccine Advisory Committee for Safe and Equitable Access, where she was the only physician and scientist, helped her learn from the other 25 members to build trust with different groups of people by listening to them. This was how she learned about what people in the community worried about, rather than operating from the perspective of what worried her.
Webb Hooper added that trust is an underappreciated social determinant of health. Trust, she said, is a complicated cognitive, behavioral, and emotional construct, and once damaged or broken, it is hard to win back. “I think the pandemic put us in a situation where because we had
not addressed long-standing distrust of a number of populations, we are now in a crisis, and we want automatic trust, and that is just not how trust works,” said Webb Hooper. She said that it is important to work consistently to earn trust by providing evidence-based information and not assuming people will believe it because it is from a scientist or physician. Rather, there has to be a dialog to understand the sources of their concerns, affirm and acknowledge what has happened previously, and convey why this time might be different. Perhaps most importantly, attitudinal change and building trust take time.
Lamas referred to the more rapid nature of trust building that has to happen in the ICU and pointed out that dealing with patient and family uncertainty is key. The willingness to acknowledge that sometimes cases are worse than expected and other times outcomes are better than expected, without saying “I do not know,” is a difficult balance to strike, she said. A particular challenge is that trust building often has to happen quickly because a decision needs to be made on the spot. Lamas shared that during the pandemic, she and her colleagues worked hard to gradually build trust with family members. However, often, that carefully developed trust eroded over time as family members began to feel that the medical staff was not trying hard enough to save their loved one or was “giving up” by asking about a transfer to hospice care.
Lamas recounted a situation with a patient who was not expected to survive; the family wanted Lamas to give their mother a medicinal supplement that they had spent a great deal of money on but that the Food and Drug Administration had identified as not effective for COVID-19. She and her team had a great deal of back-and-forth about whether to acquiesce to the demand. Ultimately, they decided to do so, essentially treating the family but providing no benefit to the patient. “This was an interesting moment of how do you build trust with people, and what does it mean if building trust means doing something that you do not actually think is useful for your patient,” said Lamas.
Webb Hooper commented that the early assumption that educating the public would be sufficient for building trust turned out in hindsight not to be the best approach, particularly since information has been changing so rapidly during the pandemic. “If the trust level is low and you give people information, they try to take that in, and then the information continues to change, it does not bode well for trust building,” she said. “That requires a much more nuanced approach to addressing trust than I think we took early on in the pandemic.”
Posing a question from the audience, Hinds asked the panel if COVID-19 is teaching us about the need to provide more information about effective treatments, such as antibody infusion. DeBiasi replied that the balance between treatment and prevention is difficult to achieve. “Most of us believe that it would be more useful and more achievable to have people vaccinated and prevent severe disease than to have full access for everyone to monoclonal antibodies once they are infected,” said DeBiasi. However, she added, “there is still going to be a subset of people who do not want to be vaccinated, and should we then deny them access to monoclonal antibodies if they get really sick? That is an ethical question.”
Lamas agreed that it is prudent for the main conversation to be about being vaccinated, and there is a tension about how much to talk about treatments that people are relying on in lieu of being vaccinated. However, people have many reasons that they choose not to receive the vaccine, so for her, the ethical decision is to treat patients with whatever means are available.
Another audience member asked the panel to comment on ethnic and racial underrepresentation in international clinical trials. Webb Hooper responded that one reason is that the distribution of race and ethnicity and even the concerns about it are different in many countries. For example, in countries such as France it is illegal to ask about race and ethnicity. Webb Hooper noted that the focus on, and categorizations of people by, race and ethnicity differs greatly compared with the United States. Other countries often focus on socioeconomic disadvantage rather than race or ethnicity, yet it remains necessary to strive for a match between trial representation and the burden of disease on specific subpopulations.
DeBiasi agreed and noted that in the trial she is conducting, her team is working to capture the patients whom COVID-19 and MIS-C are affecting the most. She explained that 85 percent of the patients in her institution are either Black/African American or Hispanic/Latinx, so focus on those populations is critical. While this may require more effort—recruiting a patient whose family only speaks Spanish, for example, requires more time and personnel than recruiting a child from a Black/African American family—it is important to dedicate the resources to achieve the proper population distribution.
Building on Lessons Learned to Guide Future Policy
To open the final session, Jon Broyles, executive director of the Coalition to Transform Advanced Care and session moderator, posed a series
of questions that he hoped the three panelists would address in their comments.
- What will it take to implement the new Center for Medicare and Medicaid Innovation (CMMI) refresh strategy as an accelerator for value-based payment models for serious illness care?
- How do we ensure health equity as part of the future of care models and payment models?
- What are some important trends that we should all be aware of that are going to impact policy moving forward from the pandemic, such as the growing presence of private equity in health care delivery and in this space in particular of serious illness?
- How will we track the trend of burnout among many frontline workers?
The Center for Medicare and Medicaid Innovation’s Strategy Refresh
Purva Rawal, chief strategy officer of CMMI, opened her remarks by explaining that the statute that created the Innovation Center explicitly provides CMS with the authority through CMMI to test innovative payment and service delivery models. The goal of developing and testing these models is to preserve or enhance the quality of care for Medicare, Medicaid, and Children’s Health Insurance Program (CHIP) beneficiaries. She specified that the models are designed to achieve one of three conditions: (1) quality improves and costs remain neutral, (2) quality remains neutral and costs are reduced, or (3) quality improves and costs are reduced. If a model achieves one of these outcomes, the Secretary of Health and Human Services (HHS) can expand its duration and scope through rulemaking.
One goal of CMMI’s “Strategy Refresh”36 is to use the last decade’s learnings to consider future directions, consider how CMMI can use the statutory mandate to develop new models, and think more broadly about its ability to affect broad system transformation. Her colleagues undertook a critical review of what CMMI had accomplished over the previous decade, which included launching over 50 models, 30 of which are still operating and a handful of which have been expanded. The team also looked to other experts across HHS and CMS and to external experts and leaders in health
___________________
36 See https://innovation.cms.gov/strategic-direction-whitepaper (accessed March 15, 2022).
policy and health care delivery to inform the refresh strategy, which it outlined in August 2021 (Brooks-LaSure et al., 2021; CMMI, 2021).
The purpose of the strategy, said Rawal, is to plot a path forward for CMMI, increase momentum toward value-based care, and reignite some of that sense of forward movement that staff felt in 2010 when CMMI first began its work. “I think there has been a little bit of a slowing down of that momentum, and maybe some not so clear signals to providers and beneficiaries about where we are headed,” said Rawal.
Other goals for the refresh strategy include taking the lessons learned over the previous 10 years to streamline and harmonize CMMI’s portfolio of models and to renew its vision to achieve equitable outcomes through high-quality, affordable, person-centered care. Rawal said CMMI has organized the strategy around five objectives: drive accountable care, advance health equity, support innovation, address affordability, and partner to achieve system transformation.
The first objective encompasses CMMI’s goal of increasing the number of people in relationships with providers who are accountable for patients’ costs and, most importantly, for improving care quality. Achieving this goal, explained Rawal, requires increasing beneficiary access to both advanced primary care and accountable care models that are equipped to coordinate the care of beneficiaries and integrate with specialty care. Accomplishing this task will ensure that the health care system is meeting the full range of patient needs.
The second objective, advancing health equity, has become one of CMMI’s most important areas of focus. It is an essential part of the strategy to improve quality, particularly for underserved populations. “We know we cannot improve quality without addressing equity up front,” emphasized Rawal. Among the strategies CMMI will employ is embedding health equity in every aspect of the models and addressing barriers to participation in the models for those providers who care for underserved or rural populations, practice in health professional shortage areas, or practice in medically underserved areas.37 As part of this effort, Rawal and her colleagues are committed to engaging a broader range of provider types, such as safety net providers, federally qualified health centers, and rural health clinics. “To achieve our accountable care goals, we know that we have to
___________________
37 See https://bhw.hrsa.gov/workforce-shortage-areas/shortage-designation (accessed March 15, 2022).
have more providers and different types of providers in our models,” she said.
To accomplish the third objective, supporting innovation, Rawal knows that CMMI can do more to support innovative care delivery approaches, which will include actionable and practice-specific data, technology, dissemination of best practices, peer-to-peer learning collaboratives, and payment and other regulatory flexibilities. Rawal pointed out that these are tools to support providers but also mechanisms for achieving the goals of better care and better outcomes for beneficiaries.
Regarding the fourth objective, addressing affordability, Rawal noted that CMMI has to be aware of the impact of a model on Medicare and Medicaid spending. In addition to reducing or stabilizing spending, these models can sometimes lower patient out-of-pocket costs, which is important for beneficiaries and their families. This is a priority across CMS, Rawal pointed out, so her team will be looking at strategies in the context of the models to target health care prices and affordability and to reduce unnecessary or duplicative care that can increase costs.
The fifth objective is furthering the reach of transformation. Rawal explained that “we want to align priorities and policies across CMS to achieve our vision, so we are working closely with our CMS colleagues, as well as with experts, beneficiaries, patient groups, payers, providers, and purchasers to achieve our vision… We know that it going to take not only a shared vision but shared commitment and action to move forward.”
Achieving these five goals will require CMMI to make key changes in how it operates. This will begin with strengthening its communications with stakeholders. The first step will be to engage with beneficiaries and advocates to integrate the patient perspective across the life cycle of the models, including during the conceptualization and development stages. CMMI also wants to gain a clearer understanding of the barriers and facilitators to participation. This will require talking to model participants and finding those that dropped out or were unable to join. “If we want to reach our goals for accountable care and advancing health equity, we are going to need to understand and address the barriers so that more folks can cross that threshold into value-based payment and then be able to sustain their participation once they are in,” said Rawal.
At the first of a long-term series of listening sessions her team held (a general session), over 1,200 participants and 15 members of the public spoke and provided comments. Rawal noted that her team is looking for additional opportunities to solicit input from experts and groups on various issues.
The second change CMMI is making is to generate and evaluate learnings from the models more dynamically, using its internal evaluation group and engaging outside experts to evaluate findings. Its data teams are piloting efforts to share research-identifiable files via the CMS Data Research Center so that researchers may link claims data with model participant lists.
Rawal said that CMMI’s “north star” would continue to be testing successful models to reduce program costs and improve quality and outcomes for Medicare, Medicaid, and CHIP beneficiaries. It also wants to review the effects that other models are having even if they do not meet the criteria for expansion, on the assumption that there may be learnings that can contribute to achieving health system transformation. Therefore, her team will be considering model success more broadly to include the following:
- how the models are affecting beneficiaries and families in terms of their patient or caregiver experiences, the quality-of-care transition, and access to home- and community-based care;
- how the models are affecting providers in terms of their ability to move down the transformation pathway;
- whether the models have an effect on providers’ administrative burden;
- whether the models are giving providers more timely and actionable data that inform care delivery; and
- whether the models have new tools or use tools differently to facilitate clinical transformation and care integration.
In addition, Rawal and her staff will be examining how the models affect health care markets, whether they are creating new linkages or relationships between providers, if they are affecting consolidation, and if successful elements of the models are spreading to other payers. “We want to define our success more broadly and think more deliberately on the front end about the potential for models to have these provider and system impacts,” said Rawal in closing.
Investing in Quality, Workforce, and Payment Models for Care of People with Serious Illness
Joe Rotella, chief medical officer of the American Academy of Hospice and Palliative Medicine (AAHPM), began with an observation about how the pandemic has shown how quickly innovation can happen, as evidenced
by the earlier presentations. He also referred to the significant challenges, such as workforce shortages, that the pandemic exacerbated and the dramatic intensification of clinician distress.
Using these observations as a launch pad, Rotella turned to the subject of the value imperative in health care and the role of serious illness care. The simplest definition of value, Rotella explained, is quality divided by cost, where quality comprises better outcomes and better experience of care. The need to focus on value and quality arises because the United States ranks last among 11 high-income nations in health care outcome and first in health care spending (Schneider et al., 2021). “Even a decade after the creation of CMMI, after moving toward value, we are still lagging,” said Rotella. “We do not see value associated with high spending.” Serious illness is part of the problem, he added, given that it is associated with poor outcomes and high costs. While numerous studies have demonstrated that palliative care improves outcomes and lowers costs, traditional fee-for-service mechanisms do not adequately fund palliative care.38
One issue with CMMI’s statutory goals is that, at the very least, the impact on costs has to be neutral, so CMMI cannot implement a model that might double quality but increase costs even slightly. Rotella said he finds it interesting that if palliative care were instead a drug that cost $500 a month, everyone with a serious illness would likely be using it today, given its proven benefits. Palliative care is a health care service, however, so it must prove that it not only improves quality of care but also can save money.
Rotella then discussed the steps toward value that Medicare—the biggest payer for people with serious illness—has taken over the past decade or so. The first was implementing the hospice benefit in 1983. Hospice has remained the gold standard for end-of-life care, care quality, and, when used appropriately, cost control. The Affordable Care Act of 2010 established CMMI, which in 2014 granted a health care innovation award to Four Seasons Compassion for Life and Duke Medical Center for its demonstration of community-based palliative care.39
Rotella explained that another important step toward value in serious illness care was the Medicare Access and CHIP Reauthorization Act of 2015
___________________
38 See http://aahpm.org/uploads/advocacy/The_Evidence_for_High-Quality_Palliative_Care.pdf (accessed March 10, 2022).
39 See https://innovation.cms.gov/innovation-models/participant/health-care-innovation-awards-round-two/four-seasons-compassion-for-life (accessed March 10, 2022).
(MACRA), which established a quality payment program for physicians:40 the merit-based incentive payment system and alternative payment models, which accelerated the move toward value. MACRA created the Physician-Focused Payment Model Technical Advisory Committee (PTAC).41 Also in 2015, CMMI launched the Medicare Care Choices model of concurrent hospice care that allowed people with cancer, heart disease, lung disease, or AIDS to pursue both hospice and disease-related treatments. It is now ending and has proven to be one of the more successful models.42
In 2018, CMS awarded MACRA funding to AAHPM and its partners, the RAND Corporation and the National Coalition for Hospice and Palliative Care, to develop palliative care quality measures to use in the quality payment program. CMMI announced several models affecting people with serious illness, including the value-based, insurance-designed hospice carve-in option in 2021.43 CMMI also announced its new strategic direction, as Rawal discussed, placed the geographic direct contracting model on hold, and decided not to go forward with a serious illness population model.
Before discussing the steps toward value by stakeholder organizations, Rotella noted that many of the efforts to increase value have focused on reducing costs, in part because quality has proven difficult to measure. To address that issue, his organization and the Hospice and Palliative Nurses Association convened the Measuring What Matters initiative to identify the best quality measures available for driving quality improvement (Dy et al., 2015). Rotella explained that most of the available measures focused on processes, and these are limited when it comes to driving quality improvement. In fact, while the United States is ranked last in health outcomes and first in spending among other industrialized nations, it is second in processes of care (Schneider et al., 2021). “We do many care processes, but we do not always see the outcomes,” said Rotella.
In 2018, PTAC recommended testing two advanced payment models, proposed by AAHPM and CTAC (Coalition to Transform Advanced Care), respectively, though Rotella noted that they are on hold or not going forward. “We still need to come up with something for the serious illness popu-
___________________
40 See https://www.cms.gov/Medicare/Quality-Payment-Program/Quality-Payment-Program (accessed March 10, 2022).
41 See https://aspe.hhs.gov/collaborations-committees-advisory-groups/ptac (accessed March 10, 2022).
42 See https://innovation.cms.gov/innovation-models/medicare-care-choices (accessed March 10, 2022).
43 See https://innovation.cms.gov/innovation-models/vbid-hospice-benefit-overview (accessed March 10, 2022).
lation,” he said. Also in 2018, the National Consensus Project44 published the fourth edition of its clinical practice guidelines for quality palliative care, calling for care coordination and some basic process of care for all individuals with serious illness. In 2019, a group of investigators published a method for identifying the serious illness population using ICD-10 (International Classification of Diseases, Tenth Addition)45 diagnostic codes and claims data (Kelley et al., 2019), which Rotella said is a great place to start to find individuals who need this intervention and measure quality.
In 2021, the Palliative Care Quality Collaborative46 launched the first unified program- and patient-level data registry in the serious illness field. In addition, the Palliative Care Quality Measures Project, which MACRA funded, submitted two patient-reported experience measures for National Quality Forum endorsement. This involved a rigorous process to focus on two patient-reported experience or outcome measures: the percentage of patients with a recent outpatient palliative care visit who report feeling heard and understood by their palliative care provider and team and the percentage who felt they were getting the help they wanted for their pain.47 The measures, which assess outcomes at the level of provider and team, fill major gaps in measuring the quality of communication and symptom management, both of which matter greatly to patients and clinicians, said Rotella. In keeping with CMMI’s new strategy, this project involved patients on the technical panel and included vigorous public engagement from over 200 stakeholders during the comment period.48
Rotella noted that the National Coalition for Hospice and Palliative Care has submitted recommendations to CMMI,49 including the following key points:
___________________
44 See https://www.cms.gov/Medicare/Quality-Payment-Program/Quality-Payment-Program (accessed March 10, 2022).
45 ICD-10-CM is a standardized classification system of diagnosis codes that represent conditions and diseases, related health problems, abnormal findings, signs and symptoms, injuries, external causes of injuries and diseases, and social circumstances. ICD-10-CM codes are required to be submitted to the payer in order for a provider to be reimbursed for services.
46 See https://www.palliativequality.org/about (accessed March 10, 2022).
47 Additional information is available at https://www.nationalcoalitionhpc.org/qualitymeasures (accessed March 10, 2022).
48 See https://www.nationalcoalitionhpc.org/qualitymeasures (accessed March 10, 2022).
49 The letter sent to the CMMI deputy director containing these recommendations is available at https://www.nationalcoalitionhpc.org/wp-content/uploads/2021/11/Coalition-CMMI-Quality-Reccs-9-24-21-FNL.pdf (accessed March 10, 2022).
- apply crosscutting structural and process requirements and quality outcome measures to all payment models that care for people with serious illness,
- build on existing work to identify the serious illness population,
- advance health care equity, and
- ensure that accountability for the quality of care for people with serious illness does not vary across payment models.
Rotella said that the specialty-level interdisciplinary palliative care workforce is insufficient for current and future needs.50 The Palliative Care and Hospice Education and Training Act51 would expand training at both the specialist and generalist levels. There is a need to study and leverage telehealth as a means of improving access to palliative care and an imperative to address systemic causes of burnout, moral distress, and inequity.
In closing, Rotella said that the Triple Aim needs to become the Quintuple Aim—better outcomes, better experiences, and lower costs sustained by thriving clinicians who deliver more equitable care. “I do not know what the future brings, but whatever surprises the future may hold, we must provide better care to people with serious illness and their families and caregivers,” said Rotella. “This was important before the pandemic, and it is even more important afterwards, when we have learned so much. We have so many tools and are poised now to make a difference, so let us double down,” he concluded.
Moving Forward
Richard Gilfillan, former president and chief executive officer of Trinity Health and the first director of CMMI, began his remarks by noting that 2 years ago, the consensus was that the nation was transforming health care. Since then, however, health care systems have had to step up and meet the incredible challenges brought on by the pandemic, yet many of them continued to do the work of transforming health care through the various models that the webinar has featured. The question is whether COVID-19 will be in the rearview mirror in a meaningful way or will remain part of the
___________________
50 See https://nap.nationalacademies.org/catalog/25789/building-the-workforce-we-need-to-care-for-people-with-serious-illness (accessed March 10, 2022).
51 See https://www.congress.gov/bill/116th-congress/house-bill/647 (accessed March 10, 2022).
health care context. “I am not sure what the answer is, but I think we have to think about it as we think about health care transformation,” said Gilfillan.
In terms of where health care is today, Gilfillan observed that accountability models, such as accountable care organizations and bundled payments, have not had any large-scale successes, but a limited test had some positive results. Gilfillan explained that tests have been hobbled by the limited commitment by providers who find that change is difficult. “No one totally turns their care model or business model upside down without a strong reason to do it, and providers have not done it yet because the need is not there,” he said. In Gilfillan’s view, a forcing function (something that makes health system leaders conclude that they must transform) is needed. Gilfillan suggested that a mandatory accountable care organization path might serve this purpose.
According to Gilfillan, any additional waivers and continuation of the waivers that have been put in place through the pandemic should only be granted in the context of providers who are actually accepting accountability for the Triple Aim or even the “Quintuple Aim.” For example, the growth in telehealth should be maintained but only in the context of providers being accountable. In addition, any activity specific to people with serious illness should be structured to be consistent with the strategic pillars of CMMI’s refresh strategy and maintain accountability. The community palliative care model is an example of a care rather than a payment model.
Gilfillan suggested thinking about how to conduct an integrated test for a model that provides care for the serious illness population, such as a team-based, community-based care model in the context of affordable care organizations. This test would explore whether this care is best delivered by a focused team or more broadly through a care management, population-based approach. His support for conducting an integrated test is based on the difficulty of providing adequate resources in that context, given the ongoing battles for resources within accountable care organizations.
Gilfillan explained that for a realistic test of a care model, CMMI needs to fund it directly and not as part of a payment model. He suggested offering this model in both the accountable care organization context and others to see if it works better in one rather than another and providing specifications for the model rather than a setting a target cost. “What we want to test is a care model, and we want to do it adequately with defined elements and a clear definition of success,” said Gilfillan. He suggested that half of the participants should be from communities that demonstrate significant health care inequities, particularly those with a lower life expectancy or other dramatically different health care outcomes.
Evaluation of the model, according to Gilfillan, should focus on whether it yields a set of outcomes that are different when delivered by a dedicated team versus by an overall kind of generalized care management approach, rather than as a test of the payment plan. “We can decide after that how to pay for it and what the payment mechanism might be. The critical point would be do we know after a year or two or three whether we start seeing evidence that this really makes a difference,” said Gilfillan.
Gilfillan pointed out that “We need to match our evaluation capabilities with the speed with which the system can change, and that is a new change that the Innovation Center and CMS as a whole need to confront. … We cannot learn in 2–5-year cycles. That is not the way to move the system forward, and we know that people in the health care system can innovate much more quickly than we thought,” concluded Gilfillan.
Discussion Session
Broyles opened the discussion session by asking Rotella to respond to Gilfillan’s suggestion about testing a dedicated care team and carving out dedicated funding versus an integrated approach. Rotella said he loved the concept and would like to explore it further. He noted that a big innovation in the Medicare hospice benefit was that it included in its conditions of participation items that are not normally part of health care spending, such as spiritual care.
Rotella pointed out the challenge of finding a basis for comparison on costs for such a model that pays for elements that fall outside the usual remit of care under fee-for-service payment. He also supported the idea that this test should be about quality of care, not cost, because it will include investments in elements outside of traditional fee-for-service health care that are essential to palliative care but currently unfunded. In addition, palliative care exists not to control costs but to give each person with serious illness the best quality of life they can have, which can sometimes, but not always, save money.
Rawal commented that she appreciated Gilfillan’s emphasis on the need for more rapid transformation and accountability, which is CMMI’s first objective in its new strategy. From CMMI’s perspective, emphasizing accountability means creating pathways for more providers to be able to engage in value-based payment and creating an imperative to move forward even if doing so is not mandatory. “How do we signal that what we want to be able to move toward is that there are accountable care entities or ways of delivering whole-person integrated care that address that full range of what patients need?” she asked.
Reflecting on the integrated model that Gilfillan discussed, Rawal said that CMMI’s teams are actively doing research on this and would welcome conversations about what has and has not worked in the accountable care organization world. A central question for her team to answer is what it looks like when there are populations that need more intensive and more specific care delivery approaches. Additionally, what are the opportunities to transform care for those populations in the context of an accountable care organization?
Broyles asked Rawal to explain why CMMI decided not to go forward with the serious illness population component of the Primary Care First model. Rawal responded that decision was based on reviewing lessons learned from the Innovation Center’s portfolio, which concluded that the risks of implementing that component as a valid test model were too high. CMS determined that the proposed outreach method for the relevant population, which was designed to comply with statutory beneficiary privacy protections, would be unlikely to result in sufficient beneficiary uptake; this low uptake would make it impossible to evaluate the model.
Rawal identified important lessons learned about beneficiary outreach and model design through which her team needs to work. She added that she hopes that her participation in this webinar signals that CMMI remains committed to seeking opportunities to develop and test value-based models of care for this population; in fact, it has several new and ongoing initiatives targeted at providing better care for such beneficiaries. Broyles noted that the number of Medicare Advantage plans with a palliative care benefit more than doubled from 2020 to 2021.
Turning to the subject of equity, Broyles asked Rawal how she views social determinants of health being addressed in CMMI’s models. Rawal replied that the overall goal is to increase the number of beneficiaries in accountable care relationships so that they get more integrated and person-centered care. Her team is exploring how this approach can include support for the social determinants of care, including greater access to home- and community-based care. “We have learned a lot from our work in the accountable health community model about how to support screening and referrals to community-based organizations,” said Rawal. “We have also learned through our primary care portfolio on how those screenings and linkages can happen.” One step will be to offer more targeted learning opportunities that would enable model participants to advance social determinants of health by working with community-based organizations to address unmet social needs.
Gilfillan commented that to address health care inequities, the current administration should commit to addressing important social determinants across the entire administration. He also challenged Medicare Advantage leaders to tell Congress they will not oppose changes to its risk adjustment that would somewhat modify the overpayments going to these plans and to take that money and put it into social services. “They are not investing in social services because they do not have the pay-fors,” noted Gilfillan. One way to pay is for Congress to apply overpayments to Medicare Advantage plans to cover social services, he explained.
In Gilfillan’s view, the current method pays providers, particularly hospital systems, extra money as a result of historical redlining.52 “To the extent that we pay Medicare rates at the same level across all communities, we are reinforcing that inequity in health care resources,” said Gilfillan. He proposed considering payment models that look at redistributing dollars in recognition of the historical impact of redlining on hospital reimbursements.
In his final comments, Rotella supported Gilfillan’s point about systemic racism reflected in the payment system. He added that it is necessary to identify the social determinants before addressing them, which requires starting with a comprehensive assessment that views people as not just health entities, but as human beings who have social lives, practical problems, and financial issues. Rotella emphasized that this is the basis of the comprehensive palliative care assessment that serves as the foundation of developing a care plan to address what matters to the individual.
Closing Remarks
To conclude the third webinar and the workshop series, Bowman explained that when the committee started planning the workshop 7 months ago, it hoped that it would be a retrospective look at the pandemic. “Now, here we are with very fresh concerns about the newest variant and the care delivery landscape that is still changing week by week, so we have been adapting and adapting at breakneck speed since March of 2020,” she said. As a result, she has the sense that the nation’s health care system will be at a
___________________
52 In the late 1930s, the Home Owners’ Loan Corporation “graded” neighborhoods into four categories, based in large part on their racial makeup. Neighborhoods with minority occupants were marked in red—hence “redlining”—and considered high-risk for mortgage lenders. See https://www.npr.org/sections/thetwo-way/2016/10/19/498536077/interactive-redlining-map-zooms-in-on-americas-history-of-discrimination (accessed March 10, 2022).
crossroads when this virus is finally under control, a theme that she felt was implicit in many conversations throughout the three webinars.
Bowman recognized so much innovation and so many new ways of caring for patients, partnering across silos, and organizing care. If such changes persist beyond the pandemic, it would represent a meaningful improvement in the lives of people with serious illness and their families. Her fear is that everyone is tired, creating the threat that the system will regress to the mean when the pandemic is over.
“As we have heard from our speakers and our patients, that is simply not good enough,” said Bowman. “Yes, patients and families are reeling from COVID, but they experienced gaps in care and unnecessary suffering before the pandemic. Yes, our health system is straining under financial burden, but it is not getting the value it could for its dollars. Providers have been stretching for years really to align with value-based care goals while having to keep a foot in the fee-for-service canoe, and our workforce is strained to the breaking point, but that need is only going to grow as the number of people living with serious illness grows.”
Adding to these challenges, she said, is the core theme throughout the workshop: the pervasive disparities in health care and health that stem from our nation’s history of racism. She said that it is difficult in the context of the pandemic not to draw the parallel that inequity is another public health emergency, one that demands the same ingenuity, the same spirit of collaboration, and the same urgency with which the nation has met the pandemic. “If, as we regroup and rebuild from the pandemic, we allow for that urgency to dissipate in our policy and our care redesign conversations, and if we do not take advantage of this opportunity, then we will have neglected the foundational principles of palliative care that each patient’s needs are unique and that every patient deserves the best that we have to offer in health care,” said Bowman.
For all of these reasons, Bowman reiterated that the main message from this webinar series is that the health care system must not regress to the mean as we emerge from the pandemic. Avoiding that, she said, is going to take strong leaders at every level who are willing to think in new ways about that system’s role on behalf of the needs of patients made vulnerable by serious illness or a history of inequity. “We need to continue to systematically scale up what was working before the pandemic, particularly expanded access to palliative care in all settings, while integrating the best of palliative care innovations and adaptations from COVID across all care delivery and all care delivery models for patients with serious illness,” she said.
In closing, Bowman said that everyone on the front line is a stakeholder in using this pandemic experience as a catalyst and an opportunity to transform care for patients with serious illness. “I am grateful to all of our speakers in this workshop because they have given us concrete strategies for pulling those COVID adaptations into the future of care delivery for patients with serious illness, for leveraging that expertise and the approaches of the palliative care field, and for holding equity as our priority.” Those strategies, she added, are the call to action, and as Rotella said in the last panel, there has never been a time with more opportunity.
Wang, in her closing reflections, noted that traditional medicine is disease centric rather than focused on the whole person or physical, emotional, social, and spiritual health. Therefore, it is natural that health care has responded to the pandemic similarly, with rapid crisis response, development of new technologies, and a hope that it will all go away. In her view, palliative medicine offers an alternate approach to not only cope with uncertainty but to cultivate hope even under severe conditions. Team-based care fosters connection, and clinicians “show up for each other,” Wang explained. “The benefit of a holistic approach addressing quality of life and supporting families is obvious,” concluded Wang, “so the compelling theme of this workshop for me is that a palliative care perspective offers solutions for our entire health system.”
REFERENCES
AACN (American Association of Colleges of Nursing). 2020. Fact sheet: Nursing shortage. Washington, DC: American Association of Colleges of Nursing.
Aiken, L. H., D. M. Sloane, L. Bruyneel, K. Van den Heede, P. Griffiths, R. Busse, et al. 2014. Nurse staffing and education and hospital mortality in nine European countries: A retrospective observational study. Lancet 3(9931):1824–1830
Ankuda, C. K., C. D. Woodrell, D. E. Meier, R. S. Morrison, and E. Chai. 2020. A beacon for dark times: Palliative care support during the coronavirus pandemic. NEJM Catalyst/Innovations in Care Delivery, May 12.
Anubui, O., T. Carter, M. Phillippi, D. G. Ruggieri, and S. Kangovi. 2021. Developing sustainable community health worker career paths. New York, NY: Milbank Memorial Fund.
Brooks-LaSure, C., E. Fowler, M. Seshamani, and D. Tsai. 2021. Innovation at the Centers for Medicare and Medicaid Services: A vision for the next 10 years. Health Affairs Blog. Washington, DC: Health Affairs.
Campos-Castillo, C., and D. Anthony. 2021. Racial and ethnic differences in self-reported telehealth use during the COVID-19 pandemic: A secondary analysis of a U.S. survey of internet users from late March. Journal of the American Medical Informatics Association 28(1):119–125.
CDC (Centers for Disease Control and Prevention). 2020. About Kawasaki disease. https://www.cdc.gov/kawasaki/about.html#:~:text=Kawasaki%20disease%20 (accessed June 9, 2022).
Chopra, S., P. Solomon, S. L. Goldhirsch, H. Fernandez, and K. Cummings. 2022. Geriatrics fellowship during COVID-19: Expanding impact, using innovation and maintaining balance. Gerontology & Geriatrics Education 43(1):55–63.
Chua, I. S., F. Zachariah, W. Dale, J. Feliciano, L. Hanson, L. Blackhall, T. Quest, K. Curseen, C. Grey, R. Rhodes, L. Shoemaker, M. Silveira, S. Fischer, S. O’Mahony, K. Leventakos, C. Trotter, I. Sereno, M. Kamdar, J. Temel, and J. A. Greer. 2019. Early integrated telehealth versus in-person palliative care for patients with advanced lung cancer: A study protocol. Journal of Palliative Medicine S1:7–19. https://doi.org/10.1089/jpm.2019.0210.
Chua, Issac, V. Jackson, and M. Kamdar. 2020. Webside manner during the COVID-19 pandemic: Maintaining human connection during virtual visits. Journal of Palliative Medicine 23(11):1507-1509. http://doi.org/10.1089/jpm.2020.0298.
CMMI (Center for Medicare and Medicaid Innovation). 2021. Innovation Center Strategy Refresh. Woodlawn, MD: Centers for Medicare and Medicaid Services.
DeBiasi, R. L. 2021. Immunotherapy for MIS-C—IVIG, glucocorticoids, and biologics. New England Journal of Medicine 385(1):74–75.
DeBiasi, R. L., X. Song, M. Delaney, M. Bell, K. Smith, J. Pershad, E. Ansusinha, A. Hahn, R. Hamdy, N. Harik, B. Hanisch, B. Jantausch, A. Koay, R. Steinhorn, K. Newman, and D. Wessel. 2020. Severe coronavirus disease–2019 in children and young adults in the Washington, DC, metropolitan region. Journal of Pediatrics 223:199–203.e191.
DeBiasi, R. L., A. S. Harahsheh, H. Srinivasalu, A. Krishnan, M. P. Sharron, K. Parikh, K. Smith, M. Bell, D. Michael, M. Delaney, J. Campos, E. Vilain, J. LoTempio, J. N. Kline, T. Ronis, S. Majumdar, E. Sadler, S. R. Conway, C. I. Berul, S. Sule, R. Lahoz, E. Ansusinha, J. Pershad, V. Bundy, E. Wells, J. E. Bost, and D. Wessel. 2021. Multisystem inflammatory syndrome of children: Subphenotypes, risk factors, biomarkers, cytokine profiles, and viral sequencing. Journal of Pediatrics 237:125–135.e118.
Dewolfe, D. J. 2000. Training manual for mental health and human service workers in major disasters. U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Mental Health Services.
Dy, S. M., K. B. Kiley, K. Ast, D. Lupu, S. A. Norton, S. C. McMillan, K. Herr, J. D. Rotella, and D. J. Casarett. 2015. Measuring what matters: Top-ranked quality indicators for hospice and palliative care from the American Academy of Hospice and Palliative Medicine and Hospice and Palliative Nurses Association. Journal of Pain and Symptom Management 49(4):773–781. https://doi.org/10.1016/j.jpainsymman.2015.01.012.
Goyal, M. K., J. N. Simpson, M. D. Boyle, G. M. Badolato, M. Delaney, R. McCarter, and D. Cora-Bramble. 2020. Racial and/or ethnic and socioeconomic disparities of SARS-COV-2 infection among children. Pediatrics 146(4).
Kane, R. L., T. Shamliyan, C. Mueller, S. Duval, and T. Wilt. 2007. The association of registered nurse staffing levels and patient outcomes: Systematic review and meta-analysis. Medical Care 45(12):1195–1204. https://doi.org/10.1097/MLR.0b013e3181468ca3.
Kangovi, S., N. Mitra, L. Norton, R. Harte, X. Zhao, T. Carter, D. Grande, and J. A. Long. 2018. Effect of community health worker support on clinical outcomes of low-income patients across primary care facilities: A randomized clinical trial. JAMA Internal Medicine 178(12):1635–1643.
Kangovi, S., N. Mitra, D. Grande, J. A. Long, and D. A. Asch. 2020. Evidence-based community health worker program addresses unmet social needs and generates positive return on investment. Health Affairs 39(2):207–213.
Katzman, J. G., K. Thornton, N. Sosa, L. Tomedi, L. Hayes, M. Sievers, K. Culbreath, K. Norsworthy, C. Martin, A. Martinez, J. Liu, and S. Arora. 2021. Educating health professionals about COVID-19 with ECHO telementoring. American Journal of Infection Control 50(3).
Kelley A. S. and E. Bollens-Lund. 2018. Identifying the population with serious illness: The “denominator” challenge. Journal of Palliative Medicine 21(S2):S7–S16. https://doi.org/10.1089/jpm.2017.0548.
Kelley A. S., K. B. Ferreira, E. Bollens-Lund, H. Mather, L. C. Hanson, C. S. Ritchie. 2019. Identifying older adults with serious illness: Transitioning from ICD-9 to ICD-10. Journal of Pain and Symptom Management 57(6):1137–1142.
Leonard, M., S. Graham, and D. Bonacum. 2004. The human factor: The critical importance of effective teamwork and communication in providing safe care. Quality & Safety in Health Care 13(Suppl 1):i85–90.
Motzer, R. J., B. Escudier, D. F. McDermott, S. George, H. J. Hammers, S. Srinivas, S. S. Tykodi, J. A. Sosman, G. Procopio, E. R. Plimack, D. Castellano, T. K. Choueiri, H. Gurney, F. Donskov, P. Bono, J. Wagstaff, T. C. Gauler, T. Ueda, Y. Tomita, F. A. Schutz, C. Kollmannsberger, J. Larkin, A. Ravaud, J. S. Simon, L. A. Xu, I. M. Waxman, and P. Sharma. 2015. Nivolumab versus everolimus in advanced renal-cell carcinoma. New England Journal of Medicine 373(19):1803–1813.
NCQA (National Committee for Quality Assurance) and Penn Medicine. 2021. Critical inputs for successful community health worker programs: A White Paper. Philadelphia, PA https://www.ncqa.org/wp-content/uploads/2021/11/Critical-Inputs-for-Successful-CHW-Programs-White-Paper-November2021.pdf.
Price-Haywood, E. G., J. Burton, D. Fort, and L. Seoane. 2020. Hospitalization and mortality among Black patients and white patients with COVID-19. New England Journal of Medicine 382(26):2534–2543.
Rock, L. K., J. W. Rudolph, M. K. Fey, D. Szyld, R. Gardner, R. D. Minehart, J. Shapiro, and C. Roussin. 2020. “Circle Up”: Workflow adaptation and psychological support via briefing, debriefing, and peer support. NEJM Catalyst Innovations in Care Delivery, September 22.
Rodriguez, J. A., J. R. Betancourt, T. D. Sequist, and I. Ganguli. 2021a. Differences in the use of telephone and video telemedicine visits during the COVID-19 pandemic. American Journal of Managed Care 27(1):21–26.
Rodriguez, J. A., A. Saadi, L. H. Schwamm, D. W. Bates, and L. Samal. 2021b. Disparities in telehealth use among California patients with limited English proficiency. Health Affairs 40(3):487–495.
Saenz, R., and C. Sparks. 2020. The inequities of job loss and recovery amid the COVID-19 pandemic. University of New Hampshire Carsey School of Public Policy. Carsey Research National Issue Brief # 150, Summer.
Schneider, E. C., A. Shah, M. M. Doty, R. Tikkanen, K. Fields, and R. D. William II. 2021. Mirror, mirror 2021: Reflecting poorly. New York, NY: The Commonwealth Fund.
Shekelle, P. G. 2013. Nurse–patient ratios as a patient safety strategy: A systematic review. Annals of Internal Medicine Mar 5:158(5 Pt2).
Stamm, B. H. 2009. Professional Quality of Life: Compassion Satisfaction and Fatigue Version 5 (ProQOL). www.isu.edu/~bhstamm or www.proqol.org (accessed March 20, 2022).
Stamm, B. H. 2010. The Concise ProQOL Manual, 2nd ed. Pocatello, ID: ProQOL.org.
Stone, R. S. B. 2018. Code Lavender: A tool for staff support. Nursing2021 48(4):15–17.
Vasan, A., J. W. Morgan, N. Mitra, C. Xu, J. A. Long, D. A. Asch, and S. Kangovi. 2020. Effects of a standardized community health worker intervention on hospitalization among disadvantaged patients with multiple chronic conditions: A pooled analysis of three clinical trials. Health Services Research 55(S2):894–901.
Vasan, A., A. Harris, S. Kangovi, and K. Mahoney. 2021. Getting proximate: Flipping the mentorship paradigm to promote health equity. The New England Jorunal of Medicine 385:24.
Webb Hooper, M., A. M. Nápoles, and E. J. Pérez-Stable. 2020. COVID-19 and racial/ethnic disparities. JAMA 323(24):2466–2467.
Yehia, B. R., A. Winegar, R. Fogel, M. Fakih, A. Ottenbacher, C. Jesser, A. Bufalino, R. H. Huang, and J. Cacchione. 2020. Association of race with mortality among patients hospitalized with coronavirus disease 2019 (COVID-19) at 92 U.S. hospitals. JAMA Network Open 3(8):e2018039.
Zhang, X., D. Tai, H. Pforsich, and V. W. Lin. 2018. United States registered nurse workforce report card and shortage forecast: A revisit. American Journal of Medical Quality 33(3):229–236.
This page intentionally left blank.
































































































